Optimized MRI Suites Enable High-Volume Turnaround, Better Access for Patients
Data collection, analytics and team synergy keys to increasing efficiencies, reducing burnout



To adapt to exponentially increasing MRI volumes, providers can implement protocol and architectural upgrades that shave minutes off exam times and make the most of every moment in the magnet.
At Mass General Brigham in Boston, Barbara Daria Wichtmann, MD, MSc, Susie Huang, MD, PhD, and colleagues had a unique opportunity of comparing the workflows at two traditional MRI facilities with those at a new facility designed to optimize patient throughput in a high-volume setting. The team presented their results during one of the scientific sessions at RSNA 2024.
“The optimized facility was recently established in one of the city’s most dynamic neighborhoods, providing a wide range of MRI services in a modern open space of campus,” Dr. Wichtmann said.
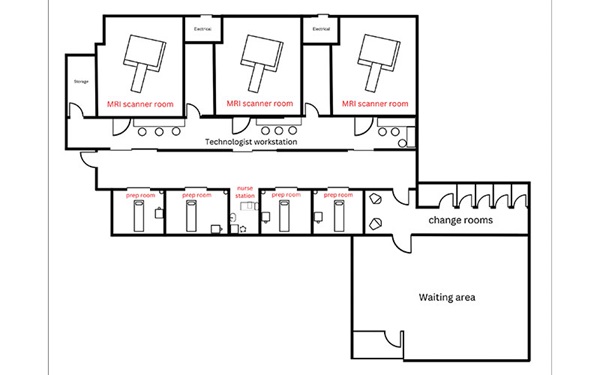
The facility features three scanners, each with two dockable tables; dedicated preparation bays located directly across the hall from each scanner, and an additional preparation bay reserved for handling potential complications or emergent events, such as allergic reactions.
While one patient is in the scanner, the next patient can be prepped in the dedicated bay—creating seamless turnover.
Dr. Wichtmann’s team retrospectively analyzed outpatient exam times and workflow for adult patients undergoing the most common brain, skull base and spine protocols from 2019 to 2024—8,434 exams in total.
All exams were performed in 3T MR scanners of the same make and model, at either the traditional or the optimized facilities. Deep learning models were used to enhance image quality, helping to reduce acquisition times.
“In the optimized facility, turnaround was reduced by up to 4.3 minutes in brain exams, 6.3 minutes for pituitary scans, 3.8 minutes for cervical spine and 2.1 minutes for lumbar spine,” Dr. Huang said. “On-time performance was significantly higher for the optimized facility, with 77% of exams starting within five minutes of the scheduled appointment, versus 50% for reference facility one and 63% for reference facility two,” Dr. Wichtmann added. “In particular, the number of examinations per scanner at the optimized facility over the observation period, exceeded the United States average by a factor of four.”

MR2025 Begins with Analytics
In 2019, at the same time the first patients were being scanned in the Mass General Brigham study, Scott Reeder, MD, PhD, was pitching a vision for the clinical MRI service at the University of Wisconsin School of Medicine and Public Health (SMPH) in Madison.
Dr. Reeder, now UW SMPH’s chair of radiology, was then the clinical chief of MRI, and faced with accommodating a rapidly increasing number of patients.
“If you’re growing at 10% per year, that means you’re doubling your volumes every seven years,” Dr. Reeder said. “It’s unsustainable to double your volume by purchasing more scanners. So, you either must add more shifts, or you need to learn to scan more efficiently, shorten your protocols and address the operational challenges that this presents.”
Enter MR2025, a strategic plan aimed to accommodate high volumes while giving patients better access to top-quality imaging services. “What we realized early on is that we had almost no data,” Dr. Reeder said. “So, our first focus was analytics—volume, access and utilization—to help us make data-driven decisions.”
Dr. Reeder’s team examined granular trends in their scan volumes, determining how many exams were performed at each site, on each scanner and in each subspecialty. The team explored how outpatient, inpatient and emergency department scheduling accommodated patients, measuring factors like the number of days until an available appointment.
Certain scans require specific conditions, such as daytime monitoring or a particular MRI strength (3T vs. 1.5T).
To prevent access gaps, scheduling must be precise, Dr. Reeder noted. Once that’s established, resource allocation such as staffing, equipment and technology, can be optimized.
Utilization was measured by tracking timestamps from the first image to the series’ end, revealing insights into the process between.
“It’s unsustainable to double your volume by purchasing more scanners. So, you either must add more shifts, or you need to learn to scan more efficiently, shorten your protocols and address the operational challenges that this presents.”
– SCOTT REEDER, MD, PHD
Focused Protocols Deliver Fast Answers
In the emergency department, a menu of targeted protocols is essential for reaching a quick diagnosis. The MR2025 plan employs focused protocols for outpatient imaging as well.
“These are fully diagnostic protocols aimed at answering a very specific question,” Dr. Reeder said.
Examples include a one breath-hold scan for diffuse liver disease—quantifying fat or iron in the liver—as well as rapid brain, spine and stroke protocols.
“We find opportunities to answer the clinical question completely, with the fewest number of sequences, to reduce exam time. When we do that, it creates more appointment slots and improves access. Patients also love it because it’s a shorter exam,” Dr. Reeder said.
The Art of Smart Architecture
In October 2024, UW Health opened East Park Medical Center, where Dr. Reeder’s team spearheaded the design of an MRI “smart suite,” inspired in part by a design implemented at NYU Langone Health. “We have two doors and two scanner tables per room. When one patient is in the magnet, the next patient is prepared on deck, ready to go,” Dr. Reeder said.
In the smart suite, room turnaround dropped from approximately 12 minutes to about two minutes—allowing the standard time slot to be reduced from 30 minutes to 20 minutes, and creating more appointment availability for patients.
“We’ve increased the number of staff to handle the rapid throughput,” Dr. Reeder said. “It’s a great environment; they’re like a SWAT team moving patients around between the systems.”
For radiologists looking to increase efficiency at their own facilities, Dr. Reeder urged thoughtful data collection and analytics to inform decisions but, especially, to lean on the strengths of the team.
“Synergy among engaged team members is incredibly empowering,” he said. “If you lay out the vision for improved efficiency and patient experience, your team’s engagement will surpass your expectations. They really want to do the right thing for the patient, and if you give them the resources and tools to do that, they will.”
For More Information
Read previous RSNA News stories about medical imaging access: