Interventional Oncology: On the Forefront of Cancer Care and Innovation
Global accreditation and advocacy are raising interventional oncology's profile in health care



Cancer is on track to outpace heart disease as the leading cause of death worldwide, and interventional oncology (IO) is positioned to meet the demand for personalized, cost-effective care.
Like interventional radiology, IO is a multidisciplinary specialty that uses minimally invasive, image-guided techniques to diagnose and treat cancer. It often leads to faster patient recovery and fewer complications while helping bridge the gap between diagnosis and therapy.
Though rapidly evolving, the field has deeper roots than many realize. “Interventional oncology is as old as the catheter,” said Michael C. Soulen, MD, professor of radiology and director of interventional oncology at the Abramson Cancer Center at the University of Pennsylvania in Philadelphia. “In the 1960s, interventional radiologists began treating cancer with chemo infusion and embolization. As image-guided therapies advanced, the field emerged as a defined clinical discipline.”
Now recognized alongside the traditional pillars of cancer care that include medical, surgical and radiation treatment, IO is also propelled by technological innovation, contributing to progress in both cancer treatment and broader areas of medicine.
“Interventional oncologists are content experts in the diseases they treat,” Dr. Soulen said. “They have a seat at the table in multidisciplinary tumor boards and disease management teams, and they provide direct and continuous cancer care from clinic to bedside.”
IO also helps bridge the gap between diagnosis and treatment.
“Multi-modality fusion guidance allows interventional oncology therapy to use imaging information (PET, CT, MRI, US, etc.) during treatment decision making to bridge diagnosis and therapy into one symphony orchestra of intelligent, highly engineered cancer care,” said Bradford Wood, MD, founding director of the National Institutes of Health (NIH) Center for Interventional Oncology, chief of interventional radiology at the NIH Clinical Center, and acting medical director, National Institute of Biomedical Imaging and Bioengineering Center for Biomedical Engineering Technology Acceleration.
As the field of IO matures, professional organizations and global initiatives are helping drive its continued growth and recognition. Organizations like the Society of Interventional Oncology (SIO) support the field through education, research funding and international collaboration. Meanwhile, new accreditation programs like the International Accreditation System for Interventional Oncology (IASIOS) are helping to standardize care and raise the specialty’s profile worldwide.

A Global Benchmark for IO Practice
Launched in 2021, IASIOS is a global accreditation initiative that promotes excellence in IO. To receive accreditation, an institution must meet the Cardiovascular and Interventional Radiological Society of Europe (CIRSE) Standards of Quality Assurance in Interventional Oncology, which are an established framework to achieve the highest standards for patient care and treatment.
Adherence to the safety and efficacy of interventional procedures involved in the management of cancer patients is also a crucial component to accreditation.
Accreditation is a multi-stage process in which institutions receive one of three distinctions: IASIOS Enrolled Centre, IASIOS Accredited Centre and IASIOS Centre of Excellence. The final seal can only be achieved when a facility is applying for re-accreditation and has held IASIOS Accredited Centre status for four years.
Raising the Bar for IO in the U.S.
As of 2025, there are over 30 IASIOS-accredited centers, with close to 30 countries represented. In 2023, the Mallinckrodt Institute of Radiology in St. Louis became the first U.S.-based institution to receive IASIOS accreditation.
Jack W. Jennings, MD, PhD, Mallinckrodt’s vice chair of procedural and clinical quality, chief of musculoskeletal radiology and director of musculoskeletal and spine interventions and procedures, was integral to the accreditation process.
Dr. Jennings explained that the continued rise of IO procedures at Mallinckrodt and throughout the medical field motivated his team to pursue accreditation to uphold the highest standards of care. “This rapid growth is seen both locally and globally, and we believe adherence to rigorous, globally agreed upon quality assurance standards is necessary for a systematic rise to enhance patients' safety and reduce medical errors, morbidity and mortality,” he said.
According to Dr. Jennings, IASIOS accreditation paved the way for many improvements at Mallinckrodt.
“IASIOS was immediately accepted by our quality and safety office and has led to improved monthly procedural/interventional oncology safety meetings with the analysis and creation of action items for addressing and preventing safety events as they relate to interventional oncology procedures,” he said.
Many of the interventional radiologists also participate on multidisciplinary tumor boards.
Standard operating procedures and IO-specific professional practice evaluations have also been developed to reduce errors and enhance safety.
“The hope is that this will also increase acceptance and credibility with both patients and referring physicians, which becomes especially important when working with other disciplines in combined therapies,” Dr. Jennings said.
While Mallinckrodt is currently the only institution in the U.S. to receive accreditation, the number of enrolled and newly accredited facilities is growing, with the National Institutes of Health in Bethesda, MD, and St. Jude Children’s Research Center in Memphis, TN, joining the ranks of enrolled centers in the U.S.
Interventional oncology will continue to develop and evolve in the future, which will include advancement in ablation planning, intra-procedural monitoring and confirmation, resulting in more standardized and reproducible ablation algorithms,” Dr. Jennings said.
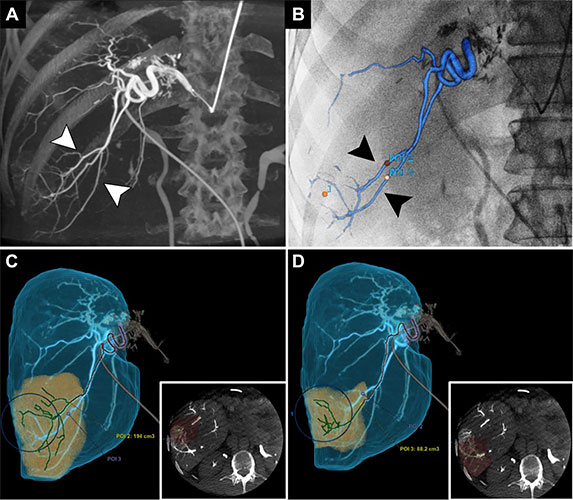
Images in a 51-year-old man with metastatic colorectal cancer to the right liver undergoing preparatory mapping angiography before yttrium 90 radioembolization. Integrated imaging software was used to delineate arterial anatomy for navigation and treatment planning. (A) Three-dimensional reconstruction generated from an intraprocedural contrast-enhanced cone-beam CT scan of the right hepatic artery shows distal arterial branches (arrowheads) supplying the region of a right liver tumor. (B) Using artificial intelligence–enabled Liver ASSIST software (GE Healthcare), vessels supplying the tumor were automatically segmented. In this image, a three-dimensional rendering of these vessels is superimposed over the fluoroscopic image, creating a three-dimensional vascular roadmap to guide microcatheter navigation (arrowheads). (C, D) Using reconstructions of contrast-enhanced cone-beam CT images, the branching pattern (green lines) and parenchymal distribution (yellow) of selected vessels are displayed.
https://pubs.rsna.org/doi/10.1148/radiol.230139 ©RSNA 2023Interventional Oncology Looks to the Future
The rapid evolution and future of IO is detailed in a commentary published in Radiology, “Interventional Oncology: 2043 and Beyond.” The authors emphasized areas of growth in the field.
“Refined ablation and endovascular techniques initially developed for liver cancer are now being applied to other areas, including the lung, brain and beyond,” they wrote. “Emerging treatments like histotripsy and electroporation are gaining traction, while combinations of interventional therapies with immunotherapy are under investigation. Researchers are also exploring intratumoral delivery of viruses and other therapeutic agents.”
Injection technologies are also experiencing some foci of excitement, according to Dr. Soulen. “Now we are using electrical pulses, focused ultrasound and viral vectors to not only destroy tumors non-thermally, but to incite a biological response in the host with the goal of enhancing control of tumors beyond the injection site,” he said.
Greater representation through IASIOS accreditation or involvement with organizations like the National Cancer Institute and the National Comprehensive Cancer Network (NCCN), which can include formal collaborations, advisory participation, research partnerships and educational initiatives, will also help drive interventional oncology forward.
Dr. Wood noted that while there is some IO representation on NCCN panels, there is still room for improvement. “Although interventional radiology and interventional oncology are becoming better represented on guideline development groups, panels and committees, they still need to have a seat at the table, or risk being on the wrong menu,” Dr. Wood said. “There is still work to be done.”
For More Information
Access the Radiology commentary, “Interventional Oncology: 2043 and Beyond.”
Read previous RSNA News stories on interventional radiology:
- Addressing the Interventional Radiology Shortage
- Interventional Radiology’s Role in Obstetrics and Gynecology
- Training Interventional Radiologists in East Africa