AI Catches One-Third of Interval Breast Cancers Missed at Screening
Algorithm correctly localizes and categorizes breast cancer, potentially reducing interval cancer rates

An AI algorithm for breast cancer screening has potential to enhance the performance of digital breast tomosynthesis (DBT), reducing interval cancers by up to one-third, according to a study published today in Radiology.
Interval breast cancers tend to have poorer outcomes due to their more aggressive biology and rapid growth. DBT, or 3D mammography, can improve visualization of breast lesions and reveal cancers that may be obscured by dense tissue. Because DBT is relatively new as an advanced screening technology, long-term data on patient outcomes are limited in institutions that have not transitioned to DBT until recently.
“Given the lack of long-term data on breast cancer-related mortality measured over 10 or more years following the initiation of DBT screening, the interval cancer rate was often used as a surrogate marker,” explained study author Manisha Bahl, MD, MPH, breast imaging division quality director and co-service chief at Massachusetts General Hospital and associate professor at Harvard Medical School. “Lowering this rate is assumed to reduce breast cancer-related morbidity and mortality.”
In a study of 1,376 cases, Dr. Bahl and her colleagues retrospectively analyzed 224 interval cancers in 224 women who had undergone DBT screening. On those DBT exams, the AI algorithm (Lunit INSIGHT DBT v1.1.0.0) correctly localized 32.6% (73/224) of cancers that were previously undetected.
“My team and I were surprised to find that nearly one-third of interval cancers were detected and correctly localized by the AI algorithm on screening mammograms that had been interpreted as negative by radiologists, highlighting AI’s potential as a valuable second reader,” Dr. Bahl said.
According to the researchers, the Radiology study may represent the first published research to specifically examine AI assistance in detecting interval cancers on screening DBT exams.
“Several studies have explored the use of AI to detect interval cancers on screening two-dimensional digital mammography exams, but to our knowledge no previously published literature has focused on the use of AI to detect interval cancers on DBT,” Dr. Bahl explained.
Improved Lesion-Level Accuracy
To avoid overestimating the sensitivity of the AI algorithm, Dr. Bahl’s team employed a lesion-specific analysis that “credits” the AI algorithm only when it correctly identifies and localizes the exact site of the cancer.
“In contrast, an exam-level analysis gives AI credit for any positive exam, even if its annotation is incorrect or unrelated to the actual cancer site, which may inflate the algorithm’s sensitivity,” Dr. Bahl said. “Focusing on lesion-level accuracy provides a more accurate reflection of the AI algorithm’s clinical performance.”
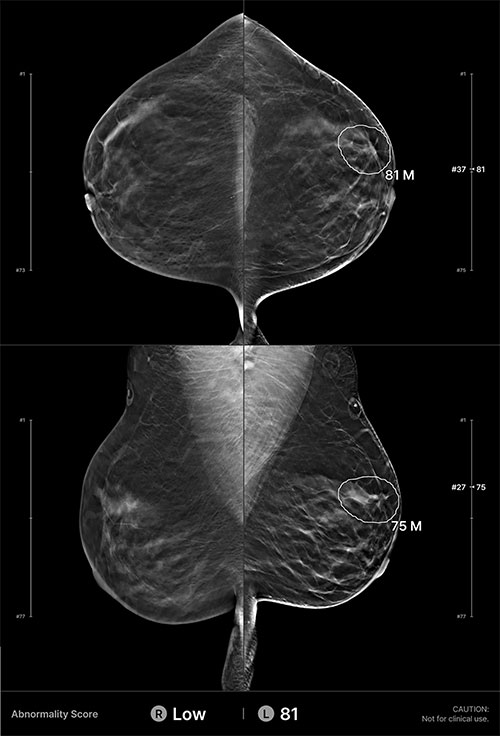
Example of an interval cancer retrospectively detected by the AI algorithm. A 41-year-old woman presented for a screening digital breast tomosynthesis examination; its findings were interpreted as negative. Ten months later, the patient presented with a lump in the left breast and was subsequently diagnosed with grade 3 invasive ductal carcinoma. At retrospective evaluation of the initial screening mammogram, the AI algorithm marked a suspicious lesion (white outline) in the left breast, with high scores of 81 on the craniocaudal view and 75 on the mediolateral oblique view. This area of architectural distortion corresponds to the cancer that was subsequently diagnosed.
https://doi.org/10.1148/radiol.241050 © RSNA 2025
Cancers detected by the algorithm tended to be larger, and they were more likely to be lymph node-positive, Dr. Bahl noted.
“These findings suggest that AI may preferentially detect more aggressive or rapidly growing tumors, or that it identifies missed cancers that were already advanced at the time of screening,” she said
Among 1,000 patients—including those with true-positive cancers based on pathology and those with true-negative and false-positive outcomes based on one-year follow-up—the algorithm correctly localized 84.4% of 334 true-positive cancers. It also correctly categorized 85.9% of 333 true-negative cases and 73.2% of 333 false-positive cases as negative.
“Our study shows that an AI algorithm can retrospectively detect and correctly localize nearly one-third of interval breast cancers on screening DBT exams, suggesting its potential to reduce the interval cancer rate and improve screening outcomes,” Dr. Bahl said. “These findings support integrating AI into DBT screening workflows to enhance cancer detection, but its real-world impact will ultimately depend on radiologist adoption and validation across diverse clinical environments.”
For More Information
Access the Radiology article, “AI to Reduce the Interval Cancer Rate of Screening Digital Breast Tomosynthesis,” and the related editorial, “Clinically Meaningful AI Detection of Interval Breast Cancer at Digital Breast Tomosynthesis Screening.”
Read previous RSNA News stories about AI in breast imaging: