Understanding Altered Brain Connectivity in Post-Concussive Visual Vertigo Syndrome
R&E Foundation grant research may identify ways to treat specific connectivity issues


In the U.S. each year, 1.6 to 3.8 million concussions occur, with up to 80% of patients experiencing acute vestibular symptoms such as dizziness, nausea, mental fog and physical imbalance. In a subset of these patients, vestibular symptoms persist beyond the acute phase, creating barriers to daily life activities and increasing costs on the health care system.
2018 RSNA Research Resident Grant recipient Anna Trofimova, MD, PhD, clinical instructor and pediatric neuroradiology fellow at Emory University School of Medicine and Children’s Healthcare of Atlanta, has completed preliminary imaging research that provides clues about the structural and functional brain connectivity involved in vestibular processing and how brain connectivity changes after mild traumatic brain injury (mTBI).
Dr. Trofimova’s research, "Functional and Structural Brain Connectivity Alterations in Visual Vertigo Syndrome: A Prospective MRI Study of Central Vestibular Impairment in Mild Traumatic Brain Injury," seeks to understand the altered brain connectivity of patients with concussion-induced visual vertigo syndrome (VVS) in order to inform patient-centered rehabilitation approaches.
“When a patient experiences vestibular symptoms on a daily basis, it can be very debilitating,” Dr. Trofimova said. “The symptoms can be provoked by any routine activities that encompass visually rich stimuli, such as going to the grocery store. Patients then require assistance with these activities, or just stop doing them altogether.”
Dr. Trofimova emphasizes that it is often assumed that patients with mTBI do not experience significant or long-term sequelae of their injuries. Also, routine structural brain MRI usually appears normal after concussion. Despite this, some patients develop persistent chronic VVS symptoms. Dr. Trofimova believes that her research will help to advance the understanding of the underlying mechanisms and explain why symptoms persist. These data could also be used for the development of personalized rehabilitation techniques. Through treatment, it may be possible to reverse vestibular impairment and prevent chronic VVS.
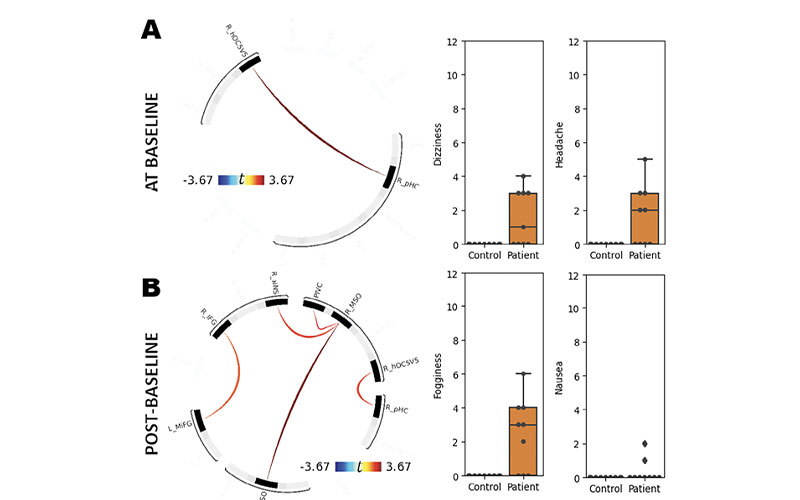
Correlations between ROI-to-ROI rs-fMRI connectivity and VOMS derivative scores. Significant correlations were found in rs-fMRI connectivity between the right posterior hippocampus (R_pHC) and right visual area hOC5/V5 (R_hOC5/V5) and VOMS baseline aggregate score (A). Significant positive correlations were also found between parieto-insular vestibular cortex (PIVC) and right multisensory orientation area (R_MSO), bilateral MSO, R_MSO, and right anterior insula (R_aINS), right inferior frontal gyrus (R_IFG) and left middle frontal gyrus (L_MiFG) and VOMS delta condition score (B). Warm colors indicate increased connectivity in correlation with increasing symptoms. VOMS, Vestibular/Ocular-Motor Screening.
Trofimova et al, Alterations in Resting-State Functional Brain Connectivity and Correlations with Vestibular/ Ocular-Motor Screening Measures in Postconcussion Vestibular Dysfunction. J Neuroimaging. 2021 Mar;31(2):277-286. Permission to publish from Journal of Neuroimaging.
Novel Vestibular Paradigm Observes Connectivity
In collaboration with her mentors, Jason W. Allen, MD, PhD, and Russell Gore, MD, and with the support of the Shepherd Centre in Atlanta and the Georgia Institute of Technology Center for Advanced Brain Imaging, Dr. Trofimova developed a novel vestibular paradigm task-based functional MRI (t-fMRI) technique to compare functional brain connectivity of patients with VVS symptoms to that of healthy controls.
The experimental group consisted of 25 patients, with subacute VVS (eight to 20 weeks after injury). The control group contained 25 age-matched healthy subjects.
During t-fMRI, participants were shown short videos portraying scenarios containing visually complex stimuli, such as a busy street in a large city, that were designed in collaboration with vestibular neurologists. These videos were interspersed randomly with videos of less visually stimulating scenery, such as a calm sea without waves.
In addition to capturing MR imaging data, the researchers also collected data from participants regarding the type of symptoms they experienced during the videos, and their severity, through the use of handheld recording devices.
In addition to the novel vestibular paradigm t-fMRI, functional brain connectivity data was captured through resting-state functional MRI (rs-fMRI) and structural connectivity data was collected through diffusion tensor imaging.
“The novel vestibular paradigm allows us to collect task-based functional brain connectivity information, as well as link each particular video to a patient’s clinical response,” Dr. Trofimova said. “Using this approach, we can track which symptoms are provoked by each video and correlate with the pattern of functional brain activation.”
She notes that healthy controls remain predominantly asymptomatic during this task, and thus the data regarding their brain connectivity is useful for comparison.
It is hoped that with enough imaging data, patients’ responses to various rehabilitation therapies may become highly predictable. This may make it possible to treat specific connectivity issues and symptoms caused by vestibular impairment with targeted rehabilitation therapies, thereby increasing positive patient outcomes and decreasing cost.
“Compared to healthy controls, patients with mTBI experience increased activity with the cortical networks involved in visual and vestibular stimuli processing.”
ANNA TROFIMOVA, MD, PHD
Preliminary Findings Promising
One interesting preliminary finding included observations regarding the vestibular system’s processing in the brain. These observations are notable because consensus does not currently exist about how vestibular information is mapped within the cortex. The researchers now have hypotheses as to the dominant hubs and nodes in the vestibular network.
“Processing of vestibular and visual stimuli is complex and involves multiple networks and cortical representations, including the parieto-insular vestibular cortex, which is considered a putative primary vestibular cortex, and also the anterior insula, frontal eye fields, hippocampi and multisensory processing areas, including the middle and inferior frontal gyri,” Dr. Trofimova said.
Another somewhat unexpected preliminary finding in the research was that the experimental group experienced increased brain connectivity between the dominant vestibular network hubs compared to the control group.
“Compared to controls, patients with post-concussive vestibular dysfunction demonstrated significantly increased rs-fMRI connectivity among vetibular network elements. In addition, rs-fMRI connectivity was significantly positively correlated with the clinical scores, which suggest that rs-fMRI brain connectivity positively predicts clinical symptom severity” Dr. Trofimova said. Dr. Trofimova and her team believe that this is because multisensory processing becomes rewired post-injury.
“This may in part be representative of altered multisensory processing causing increased weighting of visual and vestibular stimuli,” Dr. Trofimova said. “Compared to healthy controls, patients with mTBI experience increased activity with the cortical networks involved in visual and vestibular stimuli processing. In other words, symptomatic patients exert much more effort to process the same vestibular information than healthy controls.”
Research Could Help Predict Patient Outcomes
Dr. Trofimova, who received a 2021 Silver Anniversary Campaign Pacesetters Research Fellow Grant to continue her brain injury research, hopes that the findings of her research can be used to develop better tailored vestibular rehabilitation techniques and potentially predict patient treatment outcomes.
“There are patients that undergo vestibular impairment therapy who do experience recovery, and there are some who don’t improve as much as we would like,” Dr. Trofimova said. “What we are lacking at this point is understanding what exactly those therapies do to the brain connectivity. Through gathering more imaging data, could we predict from the beginning, before even applying therapy, which vestibular rehabilitation technique will be most effective as well as what the outcomes will be? That’s probably the biggest question, and we have a long journey ahead of us to try and answer that question."
For More Information
Access the Journal of Neuroimaging study, at onlinelibrary.wiley.com/journal.
Learn more about R&E Funding Opportunities.
Read previous RSNA News stories on R&E Foundation grants: