Trauma Imaging in Pregnancy: What Clinicians Need to Know
New overview covers imaging modalities, clinical considerations and best practices to support timely, accurate diagnosis

In concert with the RadioGraphics monograph, RSNA News shares the latest in emergency imaging.
Trauma is the leading cause of non-obstetric mortality in pregnant women in the U.S., with domestic violence, motor vehicle collisions and falls topping the list. To address these serious clinical scenarios, radiologists must be proficient in the treatment of pregnant patients, particularly in the emergency setting.
In a new clinical overview published in RadioGraphics, Margarita V. Revzin, MD, associate professor of radiology and biomedical imaging at the Yale School of Medicine in New Haven, CT, and colleagues offer evidence-based recommendations to support confident, timely imaging decisions in pregnant patients who have experienced trauma.
“Imaging should never be withheld from pregnant trauma patients when clinically indicated,” Dr. Revzin said. “A major misperception is the overestimation of fetal radiation risk. Clinicians often avoid ordering necessary tests out of fear, but studies have shown that most diagnostic imaging, including CT, involves radiation doses well below harmful thresholds.”
Effective interdisciplinary collaboration and clear communication with colleagues, patients and caregivers are essential, according to Dr. Revzin. She noted that resources such as RadiologyInfo.org, as well as practice parameters and technical standards provided by organizations like the American College of Radiology, can help support patient understanding and provide reassurance.
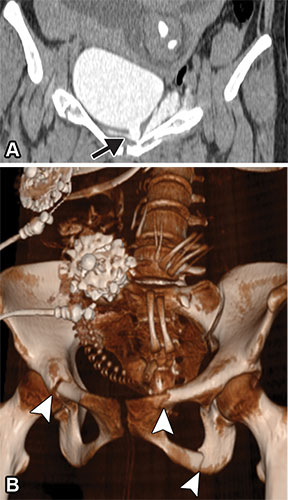
Extraperitoneal bladder rupture in a 24-year-old woman at 29 weeks of gestation after experiencing trauma. Coronal CT cystogram (A) and three-dimensional (3D) reconstruction CT image (B) show extraperitoneal extravasation of contrast material–opacified urine (arrow in A). Multiple pelvic fractures are seen on the 3D reconstruction image (arrowheads in B), in addition to the fetal skeleton. In a patient with a pelvic fracture, evaluation with cystography or delayed imaging is reasonable despite the additional radiation exposure. Attention should be given to potential fetal skull fractures (see Fig 8).
https://pubs.rsna.org/doi/10.1148/rg.240043 ©RSNA 2025
Guiding the Imaging Approach
Stabilizing the mother is always the top priority, as maternal health directly impacts fetal outcomes, Dr. Revzin said. Prior research has shown that life-threatening trauma is associated with a fetal loss rate of about 40% to 50%, and maternal shock from major injuries accounts for 80% of those losses.
“Once the mother is stable, imaging focus shifts to the fetus—assessing viability, placental integrity and any signs of distress or injury,” Dr. Revzin said. “Imaging helps us to balance rapid diagnosis with fetal safety.”
Continuous external fetal monitoring also is crucial during and after trauma evaluation to promptly identify any signs of fetal distress and facilitate timely clinical decisions.
For hemodynamically stable patients and those with suspected abdominal or pelvic injuries, focused assessment with sonography for trauma (FAST) is commonly used for the initial triage.
Complementing these early steps, safe and accessible US is the first-line modality in pregnancy. It is useful for gross uterine integrity assessment and fetal evaluation but does have limitations. “Ultrasound is great for assessment of the pregnancy itself but is limited for assessing the injuries to the mother or skeletal injuries to the fetus,” Dr. Revzin said.
According to the authors, initial US misses 50% to 80% of placental abruptions, often because the bleeding may not be detectable yet. “Just because you can’t see it doesn’t mean it’s not there,” Dr. Revzin said, adding that placental abruption is the second leading cause of fetal death after maternal shock.
“If the pregnant patient is stable, then imaging starts with bedside ultrasound to check the fetal heart rate and the placenta,” Dr. Revzin said. “Portable radiographs may be obtained to check for maternal fractures. For unstable patients or those with more severe suspected injuries, we usually go straight to CT.”
CT and MRI: Risks, Benefits and Best Uses
According to Dr. Revzin, despite involving ionizing radiation, CT is often indispensable in trauma assessment, particularly for evaluating suspected abdominal or pelvic injuries.
In a stable patient whose cognition is not impaired, Dr. Revzin noted that informed consent can be obtained and should include a discussion of radiation risks to the fetus. If necessary, consultation with a medical physicist may be considered to estimate fetal exposure. In an unstable patient, it is appropriate to proceed without formal consent.
In addition to delaying a timely and accurate diagnosis, being overly conservative—such as using ultra-low-dose protocols and no contrast CT—may increase radiation exposure if additional exams are needed. Dr. Revzin and her coauthors emphasize that intravenous iodinated contrast is considered safe to use during pregnancy and can improve detection of maternal and some fetal injuries.
MRI, though free of radiation, is not typically used in emergency settings due to its longer acquisition times. “MRI is most useful in subacute settings, and especially if there are some neurological deficits, or concerns about placental injury or insufficiency,” Dr. Revzin said.
She added that gadolinium-based contrast should be avoided unless necessary and if it is determined that the benefits outweigh the risks. “MRI is an excellent modality when time allows and the clinical picture is very complex,” Dr. Revzin said.
Gestational Age Matters: Evolving Risks and Considerations
Dr. Revzin and colleagues note that as pregnancy progresses, fetal susceptibility and maternal anatomy change. Fetuses in late pregnancy face greater risks from direct pelvic trauma. Additionally, physiological changes during pregnancy, such as increased blood volume and organ displacement, also increase maternal vulnerability to abdominal injury and complicate the diagnosis of injury.
Above all, Dr. Revzin emphasized, “Don’t delay or avoid imaging that’s clinically necessary. Protecting the mother’s health is the best way to protect the fetus.”
For More Information
Access the RadioGraphics article, “Imaging of Trauma in Pregnant Patients.”
Visit RadiologyInfo.org to find patient-friendly resources related to imaging pregnant patients.
Access the document, “ACR-SPR Practice Parameter for Imaging Pregnant or Potentially Pregnant Patients with Ionizing Radiation.”
Read previous RSNA News stories on imaging pregnant patients: