Imaging Reveals Key Patterns of Substance Abuse
CT and MRI aid in differentiating acute and chronic cardiopulmonary manifestations of drug abuse

In concert with the RadioGraphics monograph, RSNA News shares the latest in emergency radiology.
Recreational substance abuse is a leading cause of death in the U.S., according to the National Centers of Disease Control and Prevention (CDC). In 2023 alone, the agency reported over 105,000 overdose-related deaths.
This high mortality rate underscores the importance of understanding how substance abuse affects the body, particularly through its impact on vital organs. Against this backdrop, radiologists in the emergency department play an important role in the early detection of substance-related complications. Their expertise enables them to identify imaging patterns that may otherwise go unnoticed, guiding timely diagnosis and intervention.
Brandon H. Koo, MD, a fourth-year resident in the Department of Radiology at Rhode Island Hospital-Brown University Health in Providence, and colleagues authored a RadioGraphics article identifying the various imaging features and patterns related to drug use that can be seen on CT and MRI.
“The imaging sequelae of substance abuse are as varied as the types of substances being used and depends on their use duration and route of use. This article serves as a good primer for the various complications that can arise in both the emergent and chronic settings,” Dr. Koo said.
According to Dr. Koo, the two most common routes of drug use are inhalation and intravenous injection, putting a significant burden on the respiratory and cardiovascular systems.
“In many instances, a patient’s recreational substance use history cannot be easily obtained, either because the patient is too acutely ill to communicate this history, or due to the stigma surrounding substance use,” Dr. Koo said.
He emphasized that when otherwise healthy adults arrive in the emergency department with unexplained clinical symptoms or unusual imaging findings, radiologists working in these environments are uniquely positioned to identify key imaging findings and patterns that indicate acute or chronic substance abuse.
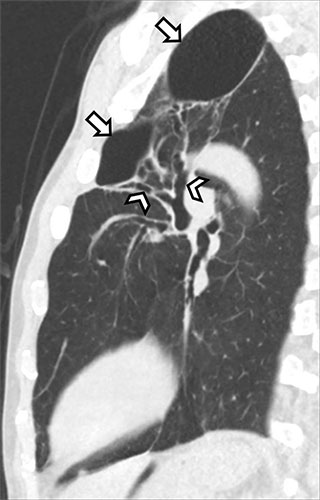
Sagittal noncontrast CT image in a 60-year-old man with a history of daily marijuana use but no reported cigarette smoking who presented with dyspnea and dry cough shows left upper-lobe bullae (arrows), with cylindric bronchiectasis (arrowheads) within a background of moderate centrilobular emphysema.
https://pubs.rsna.org/doi/10.1148/rg.250013 ©RSNA 2025
Damaging Effects of Drug Abuse Revealed
To assist radiologists in recognizing the signs of substance abuse, Dr. Koo and his coauthors highlight key imaging features and patterns of a variety of substances.
- E-cigarette use or vaping-associated lung injury (EVALI)
A spectrum of lung injury patterns is seen on CT findings of EVALI, including organizing pneumonia (OP), diffuse alveolar damage or hemorrhage, and acute eosinophilic-like pneumonia.
The authors note that most EVALI cases exhibit an OP pattern that can be further subcategorized as parenchymal-centric, airway-centric or mixed patterns of inflammation. A distinguishing imaging feature of EVALI is centrilobular ground-glass nodules, sometimes appearing in a larger panacinar form that fills most secondary pulmonary lobules.
EVALI can also be accompanied by findings of barotrauma, most commonly presenting as pneumomediastinum, with more severe cases presenting with pneumothorax.
- Marijuana
Marijuana and cigarette smokers share many imaging features, including findings of airway inflammation and emphysema. In marijuana smokers however, Dr. Koo said that a paraseptal-predominant pattern of emphysema is more often seen, as well as apical bullae that can enlarge with time, predisposing to rupture and pneumothorax.
“Most importantly, these features manifest in marijuana smokers at a younger age compared to cigarette smokers, possibly due to the higher concentration of particulates in marijuana smoke,” he added.
- Cocaine
Inhalation of crack cocaine can manifest as acute pulmonary injury with bilateral parenchymal consolidations, often referred to as “crack lung.” Dr. Koo emphasized that the prothrombogenic effects of cocaine can also result in superimposed pulmonary embolism seen as filling defects within the pulmonary arteries.
He added that cocaine is also associated with a host of cardiovascular complications, including coronary vasospasm, myocardial infarction (MI), myocarditis and cardiomyopathy, for which cardiac MRI plays a crucial role in diagnosis.
- Methamphetamine
Methamphetamine users share many of the same cardiovascular complications as cocaine users. Prior research demonstrated subendocardial late gadolinium enhancement in methamphetamine users in the absence of obstructive coronary disease, suggesting that vasospasm may also be a causative factor in methamphetamine-induced MI.
As in the case of chronic cocaine use, long term methamphetamine use has been linked to dilated cardiomyopathy and progressive heart failure.
- Intravenous Drug Use (IVDU)
A contributing factor of IVDU-related mortality is the high rate of unsafe injection practices, such as the use of nonsterile drugs and sharing needles, resulting in infectious endocarditis, septic pulmonary emboli and related complications.
Dr. Koo and colleagues point out that electrocardiographically-gated CT angiography (CTA) offers similar sensitivity to transthoracic echocardiography in detecting valvular disease. Gated CTA provides clearer delineation of perivalvular infection, which appears as areas of low attenuation nonenhancement surrounding the valve annulus and is an indication for surgical intervention.
- Opioid Use
The most common complication of opioid overdose is aspiration, which can lead to aspiration pneumonitis and/or pneumonia. Reversal of overdose with an opioid antagonist like naloxone frequently induces vomiting, further increasing aspiration risk.
On imaging, aspiration typically appears as bilateral, dependent consolidative opacities, along with intraluminal airway debris throughout the tracheobronchial tree.
Even when bradypnea resolves after the acute phase of opioid intoxication, patients may still exhibit prolonged hypoxia secondary to opioid-induced or naloxone-induced noncardiogenic pulmonary edema. Dr. Koo said that imaging often reveals interlobular septal thickening and ground-glass opacities, frequently seen on top of pre-existing lung damage caused by aspiration.
- Intravenous Excipient-related Lung Disease
Grinding prescription pills and dissolving them for injection introduces insoluble excipients into pulmonary vessels and results in a granulomatous reaction, referred to as excipient lung disease (ELD).
ELD is characterized at CT by the presence of diffuse pulmonary micronodules, which correspond to perivascular granulomas in a centrilobular pattern. Over time, these nodules can ultimately coalesce and progress towards fibrotic lung disease.
A less common subtype of ELD is also discussed in the setting of methylphenidate abuse, which presents uniquely on imaging as panlobular emphysema, which can mimic alpha-1-antitrypsin deficiency.
Efforts Towards Drug Cessation
Dr. Koo emphasized that radiologists play a crucial role in the timely identification of patients suspected of recreational substance abuse, connecting them to appropriate care and resources for long-term recovery. Ultimately, this can help prevent progression to more chronic forms of substance abuse related cardiopulmonary injury including pulmonary fibrosis, emphysema, cardiomyopathy and pulmonary hypertension.
The role of radiologists, however, does not end in the ED setting, with many patients initially presenting with acute intoxication often returning for follow-up imaging.
“Being informed of what kind of rehabilitation and care these patients received in the interim, or lack thereof, is crucial in understanding any changes in their follow-up imaging and whether these imaging findings resolve or progress with time,” Dr. Koo said.
For More Information
Access the RadioGraphics article, “Recreational Drug-induced Cardiopulmonary Injury.”
Read previous RSNA News stories on drug-related illness: