Spotting Critical Cardiac Clues on Emergency Chest CT
Radiologists can implement a structured checklist to prevent missed cardiac diagnoses

In concert with the RadioGraphics monograph, RSNA News shares the latest in emergency imaging.
Nongated chest CT exams are frequently ordered in the emergency department (ED) to evaluate for pulmonary embolism, pneumonia or trauma. Each scan also images the heart. Overlooking the heart in these studies can mean missing potentially life-threatening cardiac abnormalities, according to the authors of a new RadioGraphics article.
“Cardiac abnormalities are often overlooked on ED chest CTs obtained for other indications, such as pulmonary embolism. Yet cardiac and noncardiac presentations frequently overlap and the management pathways differ,” said lead author Kate Hanneman, MD, MPH, from the Department of Medical Imaging at the Temerty Faculty of Medicine, University of Toronto and University Health Network in Toronto. “We aimed to provide a practical, systematic guide to help radiologists, regardless of subspecialty, identify acute non‑traumatic cardiac abnormalities that can change patient care and outcomes.”
Missed Findings in Routine Practice
While exact data on miss rates are limited, cardiac findings are commonly overlooked on emergency chest CT, particularly when attention is focused on a suspected noncardiac diagnosis. “Building in a brief, structured evaluation of the heart at the end of every ED chest CT interpretation can improve detection,” Dr. Hanneman said.
She and her coauthors emphasize that the implications of a missed diagnosis can be severe. Acute cardiac conditions—including myocardial infarction (MI), spontaneous coronary artery dissection (SCAD), aortic root dissection with coronary extension, and pericardial tamponade—can present with nonspecific symptoms such as chest pain, dyspnea or palpitations. Identifying related imaging findings early can directly alter patient management and improve outcomes.
For example, the team describes cases in which timely recognition of pericardial tamponade or coronary dissection on nongated chest CT prompted urgent intervention, changing the course of treatment and potentially saving lives.
Role of Noncardiac Radiologists
Dr. Hanneman noted that most ED chest CTs are interpreted by noncardiac-trained radiologists. She emphasized their role as critical first responders in identifying potential cardiac emergencies. “Their review of the heart is a critical first chance to flag a potential cardiac emergency,” she said.
Even when findings are subtle or uncertain, clear communication with the referring clinician can prompt confirmatory imaging or additional testing, leading to faster diagnosis and treatment.
Cardiac motion and contrast phase can limit the sensitivity of nongated CT for some specific findings. Dr. Hanneman said faster scanners and multiplanar reformatting can help improve visualization. Window settings should be adjusted to optimize differentiation between normal myocardium and areas of low attenuation suggestive of ischemia or edema.
“It is important to acknowledge limitations of cardiac evaluation on non-dedicated imaging and communicate certainty of findings and need for confirmatory evaluation as appropriate,” Dr. Hanneman said.
Radiologists should also correlate imaging findings with the available clinical data, including electrocardiography and troponin levels, to guide interpretation, she added.
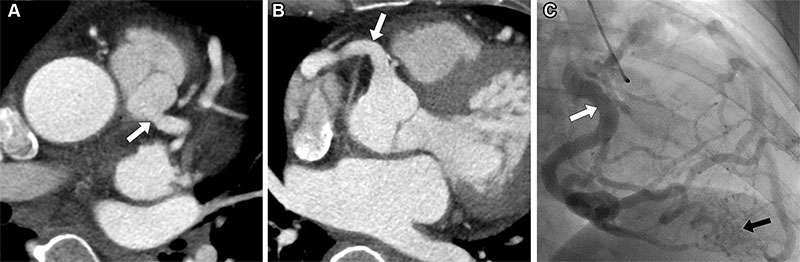
Anomalous left coronary artery from the pulmonary artery in a 50-year-old woman who presented to the emergency department with chest pain. (A, B) Axial intravenous contrast-enhanced chest CT images show an anomalous origin of the left main coronary artery arising from the main pulmonary artery (arrow in A) with coronary dilatation and a dilated right coronary artery (arrow in B) due to collateral vessel supply to the myocardial territory by the left main coronary artery. (C) Invasive catheter coronary angiogram acquired one week later shows tor[1]tuosity and dilatation of the right coronary artery (white arrow) giving rise to collateral vessels that supply the left main coronary artery territory (black arrow).
https://pubs.rsna.org/doi/10.1148/rg.250001 © RSNA 2025
Building Confidence in Cardiac Assessment
Many radiologists feel less confident evaluating the heart on nongated scans. Dr. Hanneman advises adopting a consistent approach and reviewing relevant teaching cases to build comfort over time.
“Consider use of a checklist and implement a standard and consistent approach to reviewing the heart on CT,” she said. “Review relevant cases in teaching files and correlate with other investigations and imaging findings on other modalities if available.”
To help radiologists avoid missing these findings, Dr. Hanneman and colleagues developed a practical checklist by reviewing cases with missed or delayed diagnoses. “Organized as a quick anatomic sweep, the checklist promotes standardized review, so important abnormalities aren’t overlooked,” she said. The checklist proposed by the authors includes:
- Coronary arteries – look for luminal occlusion, dissection flaps or abnormal origins
- Cardiac chambers – assess size, wall thickness or thrombi
- Myocardium – evaluate for hypoattenuation, edema or signs of ischemia
- Pericardium and pericardial fat – check for effusion, thickening or fat necrosis
- Central vessels – note aortic root abnormalities or extension of dissection
The article also includes a summary table categorizing findings by urgency. Urgent processes include acute MI, coronary dissection, pericardial tamponade and aortic root dissection.
Moderately urgent findings include pericarditis, myocarditis, endocarditis and cardiac thrombi. Nonurgent but clinically relevant findings include anomalous coronary artery origins, pericardial fat necrosis and cardiomyopathies.
In addition, the article highlights several imaging tips:
- Don’t dismiss hypoattenuation of the myocardium—this may indicate acute MI even when the scan was not ordered for cardiac evaluation.
- Check for right heart strain on scans evaluating pulmonary embolism, as this can impact management decisions.
- Report coronary artery calcification when visible, as it may influence long-term cardiovascular risk assessment.
- Assess the pericardium carefully for effusion, enhancement, or fat necrosis, which can mimic other acute thoracic conditions.
The message to radiologists is clear: all thoracic imaging scans include the heart, and a brief structured review can detect urgent cardiac findings that may affect patient outcomes.
“Always review the heart on every ED chest CT, especially when no other cause to account for the patient’s presentation is identified,” Dr. Hanneman said.
“By integrating this checklist approach into daily practice, radiologists can improve detection of life-threatening cardiac conditions—even when the scan wasn’t specifically ordered for cardiac evaluation—and ensure patients receive timely, appropriate care,” Dr. Hanneman concluded.
For More Information
Access the RadioGraphics article, “Cardiac Imaging Findings at Nongated Chest CT in the Emergency Department.”
Read previous RSNA News stories about cardiac imaging: