AI Tools Can Aid in Identifying Incidental Findings
Workflow changes, application, integration and implementation among key considerations


This is the second in a series of articles about radiologists’ role in the identification and communication of incidental findings. Read the first and third articles in the series.
AI tools designed to identify clinically significant incidental findings—those findings that are unrelated to the original purpose of an imaging exam—may expedite the diagnosis and treatment of a variety of conditions.
Recent research has uncovered the types of incidental findings that AI tools are most effective at detecting, offering insight into how these tools impact radiologist workloads and radiologists’ perceptions of this technology.
Diagnosing Critical CT Findings
Incidental findings are a common occurrence on CT scans. AI tools have shown potential in quantification, risk estimation and prioritization of critical findings.
In a study published in Radiology: Cardiothoracic Imaging, Laurens Topff, MD, a radiologist at the Netherlands Cancer Institute, and colleagues evaluated the diagnostic efficacy of one such tool in detecting incidental pulmonary embolisms (IPE) in cancer patients.
“These clots are often found incidentally when scanning for other reasons,” Dr. Topff said.
The AI tool used in the study achieved a high level of diagnostic accuracy of IPE with a sensitivity of 91.6%. By flagging critical findings, the AI tool substantially reduced diagnosis times for a backlog of unreported scans.
“When we added the AI tool to mark suspicious scans as high priority, the time to diagnosis was reduced from days to just one hour,” Dr. Topff said. “This means patients can receive potentially life-saving treatment much faster. The AI tool was very accurate and detected pulmonary embolisms that were initially overlooked by radiologists.”
In a separate Radiology study focused on extrapulmonary incidental findings and mortality prediction on chest CT in lung cancer screening, the team demonstrated that a fully automated AI tool with multi-structured segmentation could accurately identify a broad spectrum of high-risk extrapulmonary features as well as mortality risk with a high degree of accuracy.
The authors emphasized that although AI tools can identify high-risk features, radiologists still need to review the clinical relevance of the findings to ensure precise care.
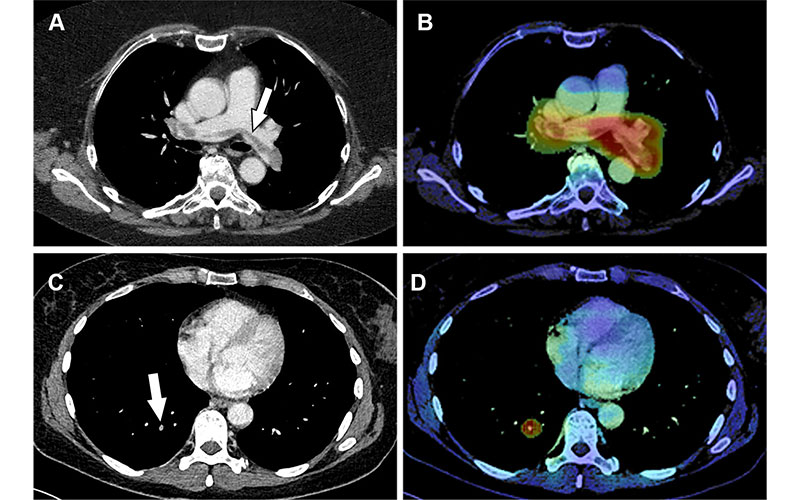
True-positive detection of incidental pulmonary embolism (PE) by the artificial intelligence (AI) software. (A, B) Images in a 68-year-old woman who underwent routine CT with intravenous contrast agent for outpatient follow-up of melanoma. (A) Axial CT image shows a large filling defect straddling the bifurcation of the pulmonary trunk (arrow) and extending into both pulmonary arteries, compatible with an incidental saddle PE. (B) Corresponding AI heatmap highlights the detected abnormality (red), thereby prioritizing the case in the radiologists’ worklist. (C, D) Images in a 58-year-old woman with a history of rectal cancer undergoing outpatient follow-up. (C) Axial restaging CT image with intravenous contrast agent shows a small incidental subsegmental PE in the right lower lung lobe (arrow). (D) Corresponding AI heatmap enables the radiologist to localize the finding (red).
Optimizing Radiologist Workflow
As AI continues to demonstrate diagnostic value, its role in streamlining radiologist workflow is becoming an equally important focus.
“The AI tool doesn’t intrinsically reduce workload. Instead, it optimizes workflow by intelligently prioritizing cases with critical findings,” Dr. Topff said. “Radiologists still review all cases, but those flagged by the AI receive earlier attention.”
Low false positive rates also limit unnecessary interruptions, enabling radiologists to focus on clinically significant findings.
“The technology complements radiologists’ expertise rather than replacing it, allowing them to allocate their attention more effectively while maintaining diagnostic responsibility,” Dr. Topff noted.
The clinical impact of these AI tools was recently examined in a study published in Radiology which evaluated whether an AI triage system could improve radiologist performance and reduce turnaround times for pulmonary embolism diagnosed by CT pulmonary angiography.
In this study, AI results were displayed via a widget interface concurrently on all workstations during image evaluation and reporting. While the AI triage system modestly improved wait times for exams with incidental findings, it did not improve diagnostic accuracy. In fact, radiologists working without AI achieved higher accuracy in detecting pulmonary embolism compared to AI alone.
The authors concluded that simply displaying AI results in a widget may not be enough. Deeper integration—such as embedding AI findings directly into the radiologist’s worklist—may be necessary to truly optimize the image interpretation workflow.
Perceptions Impact Successful AI Implementation
Beyond streamlining operations, the broader success of AI tools in radiology also hinges on how radiologists perceive and engage with these technologies.
One approach that seeks to leverage the information obtained from incidental findings is opportunistic screening. AI can help maximize the value of these imaging tests.
“Opportunistic screening is the detection and result messaging of clinically actionable radiologic findings, whereas incidental findings connote all imaging findings that may or may not have any change in medical management but are noted for the sake of completeness,” said Katherine P. Andriole, PhD, associate professor of radiology at Harvard Medical School, Brigham and Women’s Hospital in Boston.
Dr. Andriole is senior author of a Clinical Imaging article, “AI implementation: Radiologists’ perspectives on AI-enabled opportunistic CT screening,” in which she and colleagues sent a survey to radiologists to assess their perceptions of AI tools and opportunistic screening.
“While 68% of radiologists were already using AI applications, only 52% were somewhat familiar with opportunistic screening,” Dr. Andriole said.
Most survey respondents indicated that opportunistic screening output requires radiologist oversight/signoff and should be included in a separate “screening” section of the radiology report. Many of them (28%) said that they would be willing to spend from one to three minutes reviewing AI-generated opportunistic screening output, while 18 % would not spend any time.
There is still some hesitancy regarding AI tools among members of the specialty, Dr. Andriole noted. “Radiologists may be hesitant to adopt AI technology due to a change in their workflow or increase in time to do their work—particularly if the technical implementation of the tool is poorly integrated into current radiologists’ systems,” she said.
Dr. Topff agreed, emphasizing the importance of identifying where these tools would be best used. “The benefits of this AI-based prioritization are most relevant in institutions facing longer report turnaround times. Implementation requires careful monitoring to ensure reliable operation of the AI-based analysis,” he said.
For More Information
Access the Radiology: Cardiothoracic Imaging article, “Artificial Intelligence Tool for Detection and Worklist Prioritization Reduces Time to Diagnosis of Incidental Pulmonary Embolism at CT.”
Access the Radiology article, “AI for Multistructure Incidental Findings and Mortality Prediction at Chest CT in Lung Cancer Screening.”
Access the Radiology article, “Prospective Evaluation of AI Triage of Pulmonary Emboli on CT Pulmonary Angiogram.”
Access the Clinical Imaging article, "AI Implementation: Radiologists' perspective on AI-enabled opportunistic screening."