Deep Learning Reconstruction Can Lead to Better Image Quality and Increased Detection of Prostate Cancer
DLR offers higher signal-to-noise and contrast-to-noise ratios for prostate diffusion-weighted images

Note: This story is part of an RSNA Special Focus section on men's health.
Multiparametric MRI is widely used to detect, localize and stage prostate cancer. However, because some prostate cancers can be subtle, being able to image at higher b values could improve their conspicuity and detection. The b-value reflects the strength and timing of the gradients used to generate diffusion weighted images (DWI), with a higher b-value resulting in stronger weighting of diffusion effects.
According to the Prostate Imaging Reporting and Data System (PIRADS), using acquired or computed DWI with a b value of 1400 sec/mm2 or higher is recommended to improve the conspicuity of clinically significant cancers. However, at around the 2000 sec/mm2 mark, image quality begins to deteriorate. With the hope of finding the opportune intersection of increased detection and better image quality, some vendors have turned towards deep learning reconstruction (DLR).
“DLR is a newly developed, artificial intelligence-based construction algorithm for MRI and CT,” said Yoshiharu Ohno MD, PhD, professor of radiology and chief of the Joint Research Laboratory of Advanced Medical Imaging at Fujita Health University School of Medicine in Japan and corresponding author of a recent Radiology study on the topic.
While DLR shows promise for image denoising and improving image quality, its impact on diffusion-weighted imaging of the prostate has not yet been assessed.
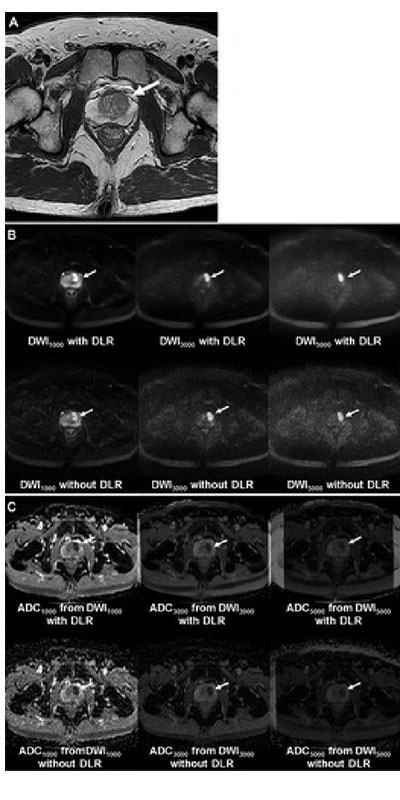
Images in a 51-year-old man with left transition zone prostate cancer. (A) T2-weighted MRI scan shows hypointense 2.1-cm prostate cancer (arrow) in the left transition zone. (B) MRI scans from diffusion-weighted imaging (DWI) with a b value of 1000 sec/mm2 (DWI1000), DWI with a b value of 3000 sec/mm2 (DWI3000), and DWI with a b value of 5000 sec/mm2 (DWI5000) with or without deep learning reconstruction (DLR). The cancer shows high signal intensity (arrows). (C) Apparent diffusion coefficient (ADC) maps obtained from DWI1000, DWI3000, and DWI5000 (ADC1000, ADC3000, and ADC5000, respectively) with or without DLR. The cancer shows low signal intensity on all ADC maps (arrows).
Ueda et al, Radiology 2022; 000:1–9 ©RSNA 2022
Image Quality of DWI Could Benefit from DLR
In the Radiology study, Dr. Ohno and his colleagues set out to determine whether the use of DLR could improve the image quality of DWI at various b values in patients with prostate cancer. To do this, the study obtained images at DWI with b values of 0 sec/mm2, 1000 sec/mm2 , 3000 sec/mm2 , and 5000 sec/mm2.
The images came from 60 patients with biopsy-proven cancer and were reconstructed both with and without DLR. Image quality was also assessed using signal-to-noise ratio (SNR) and contrast-to-noise ratio (CNR). Apparent diffusion coefficients (ADCs) from DWI with and without DLR were also compared.
Based on this work, researchers found that DWI with DLR showed significantly better SNRs and CNRs than DWI without DLR. Furthermore, DWI with DLR also demonstrated better qualitative image quality than DWI without DLR.
“Deep learning reconstruction improves the image quality of diffusion-weighted MRI scans for prostate cancer with no impact on apparent diffusion coefficient quantitation using a 3.0-T MRI system,” Dr. Ohno said. “This confirms DLR’s potential for improving lesion characterization in patients with suspected prostate cancer.”
The study also found that ADCs derived with and without DLR did not differ substantially This is critical to ensuring that DLR does not insert confounding features into the images. The area under the curve of ADC from DWI with a b value of 3000 sec/mm2 with DLR was significantly higher than that of ADC from DWI with a b value of 1000 sec/mm2 and without DLR. In addition, the sensitivity and accuracy of DWI with a b value of 3000 sec/mm2 with DLR were significantly higher than those of others.
“Traditionally, when using MRI to detect prostatic cancer without the benefit of DLR, imaging performance has been limited to 2000 sec/mm2 or less–the result of trying to maintain image quality,” Dr. Ohno said. “However, what our study shows is that, with the addition of DLR, a DWI with 3000 sec/mm2 can be used, giving routine clinical practices the ability to significantly improve diagnostic performance.”
Based on the thesis that applying DLR to DWI with 3000 sec/mm2 may have the potential to improve prostatic cancer detectability and PIRADS evaluation, Dr. Ohno next plans to directly compare DWIs with 3000 sect/mm2 with DWIs between 1400 and 2000 sec/mm2 .
For More Information
Read previous RSNA News articles on men's health:
- The Role of Imaging in Diagnosing Erectile Dysfunction
- Imaging of Testicular Germ Cell Tumors
- Ultrasound Technique Treats Prostate Cancer with Minimal Side Effects
Mobile Prostate Cancer Screening Units Increase Access to Care
To increase access to prostate cancer screenings and reach communities with higher incidence of the disease, mobile prostate cancer screening units are providing important outreach throughout the U.S.
Many of the mobile units offer prostate-specific antigen tests, digital rectal exams, US and genomics testing. Staff on-board can also assist with scheduling additional screening appointments or follow-ups with local hospitals or medical clinics.
To support prostate health in areas where prostate cancer disproportionately affects a certain population, many units focus on outreach in these areas. Prostate cancer is twice as common in Black men as it is in Caucasian men. Black men also have a twofold higher mortality rate from the disease. Therefore, many mobile units focus on care in Black communities.
Other mobile units affiliated with hospitals, universities or nonprofit groups drive throughout the country partnering with local events, churches, businesses and community groups to raise awareness of the disease and the importance of early detection.