Hyperpolarized MRI Improves Lung Disease Classification
New non-invasive imaging can assess disease activity, progression and therapy response


New research, funded by the R&E Foundation, shows that advanced MRI can quickly, accurately and non-invasively triage patients with lung disease, potentially speeding the onset of life-saving treatment.
Interstitial lung disease (ILD) refers to a large group of diseases that cause scarring in the lungs. The most common ILD is idiopathic pulmonary fibrosis (IPF), a progressive condition that leads to problems with breathing. Patients with IPF face a poor prognosis, with a mean survival of just a few years.
“Unfortunately, a lot of these patients present very late in the cascade of pulmonary fibrosis to the point where they have minimal treatment options,” said Joseph Mammarappallil, MD, PhD, assistant professor of radiology at Duke University School of Medicine in Durham, NC. “Many of them are placed on the list for a lung transplant.”
Diagnosis of IPF relies heavily on CT, which provides information on lung structure, but nothing about function. Early fibrotic lung disease may look like other ILDs such as non-specific interstitial pneumonia (NSIP) on CT. While new anti-fibrotic drugs have demonstrated benefits in reducing the progression of IPF, treatment may be delayed by missed diagnosis. Additionally, these patients often must undergo a high-risk surgical lung biopsy to assist with diagnosis.
“Diagnosing ILD is a big challenge for us as chest radiologists because there are different diagnoses that all have different treatment algorithms,” Dr. Mammarappallil said.
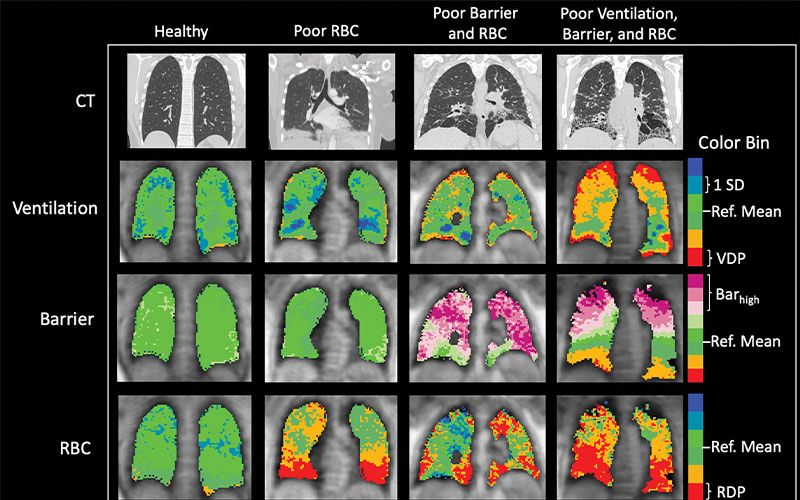
Representative CT scans, xenon 129 (129Xe) MRI ventilation scans, barrier scans, and red blood cell (RBC) scans in healthy control participant and three participants with nonspecific interstitial pneumonia (NSIP) and range of findings (from left to right: man, age 24 years; woman, age 46 years; woman, age 55 years; and woman, age 57 years). Orange and red indicate reduced signal in ventilation and RBC components, indicating abnormalities. Purple indicates increased signal in barrier component, possibly indicating thickened barrier and/or fibrosis. The first and third scans in participants with NSIP (second and fourth columns in figure) show common pattern of basilar-predominant RBC transfer defects. Note that although these RBC transfer defects are ubiquitous features in participants with NSIP, some participants with NSIP have preserved, normal-looking barrier uptake and/or ventilation. Regional correspondence is visible between CT and 129Xe MRI abnormalities. Notably, regions of high barrier measured using 129Xe MRI are also associated with normal CT findings, suggesting early-stage microstructural disease activity not yet visible on CT scan. Barhigh = high barrier percentage, Ref. = reference, RDP = red blood cell defect percentage, SD = standard deviation, VDP = ventilation defect percentage.
Mummy et al, Radiology 2021; 301:211–220 ©RSNA 2022
Polarized Xenon Gas Helps Radiologists Evaluate Gas Exchange
Dr. Mammarappallil and his colleague Bastiaan Driehuys, PhD, a physicist and professor of radiology at Duke, have been working to improve IPF diagnosis through hyperpolarized (HP) 129Xe MR imaging of the lungs. In the procedure, patients inhale polarized xenon gas before undergoing an MRI scan. The xenon allows doctors to evaluate gas exchange through several biomarkers.
“As radiologists watching the MRI in live time, we get a specific signal in the air spaces. Then, we get another one when the gas transits the basement membrane of the lungs to go to the red blood cells and then we receive another signal when it gets to the red blood cells,” Dr. Mammarappallil said. “In the case of specific diseases, these signals will be poor.”
Dr. Mammarappallil received a 2018 Bracco Diagnostics Inc/RSNA Research Scholar Grant to help fund his research into specific lung disease signatures based on HP MRI. The study, published last year in Radiology, compared 36 participants with NSIP and 15 healthy controls. Results supported the technology’s potential, showing that participants with NSIP had a higher barrier signal uptake and an increased red blood cell transfer defect.
“Hyperpolarized MRI tells us that because of the structural abnormalities of NSIP, the gas is stuck in the basement membrane and barely getting to the red blood cells,” Dr. Mammarappallil said. “We get a specific signature with IPF, with NSIP and with end-stage fibrosis that looks different than the signature of someone with normal lungs.”
HP MRI with xenon figures to be an important adjunct in the diagnostic workup of patients with lung disease, Dr. Mammarappallil said. He noted that pulmonary fibrosis patients often do poorly despite no changes in follow-up CT scans.
“However, when we image those patients with xenon gas, we often see significantly decreased gas exchange compared to the previous MRI,” he said. “We’re actually getting to the physiology of gas exchange with this technique.”
R&E Grant Helps Identify Other Areas of Research
The R&E Foundation grant helped Dr. Mammarappallil expand his research group and begin developing other applications for xenon gas MRI. The grant also led to an internal grant supporting his group’s study of machine learning to look at different xenon MRI signatures in IPF and NSIP.
In addition, the research team was able to use the grant to launch the first evaluation of people with chronic pneumonitis, a large group of pulmonary fibrosis patients who have not been studied in this manner before. Dr. Mammarappallil expects to publish those results shortly.
Dr. Mammarappallil’s team continues to add patients to its research pool as they work to develop specific signatures not just for the different disease groups but also for pulmonary fibrosis itself.
“The big thing I can see ahead is using xenon MRI to identify the earliest stages of pulmonary fibrosis,” he said. “That’s my next goal and that’s what my next round of funding is going to allow for me.”
For More Information
Access the Radiology study, “Hyperpolarized 129Xe MRI and Spectroscopy of Gas-Exchange Abnormalities in Nonspecific Interstitial Pneumonia."
Read previous RSNA News articles about R&E Foundation grants: