More Breast Cancers Found with Combined Digital Screening
Researchers caution about clinically irrelevant detection with the high-sensitivity of DBT

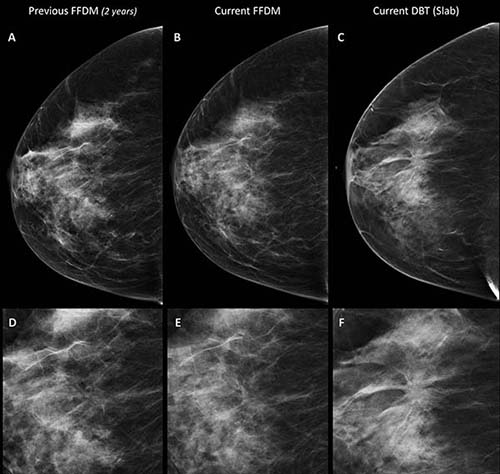
A combination of digital mammography and tomosynthesis detects 90 percent more breast cancers than digital mammography alone, according to a new study in Radiology.
To learn more about the impact of digital breast tomosynthesis (DBT) on sensitivity and recall rate, researchers compared results between 9,777 women randomized to undergo digital mammography and DBT and 9,783 randomized to have digital mammography alone.
The combination of digital mammography and DBT detected 8.6 cancers per 1,000 cases, a rate almost twice that of the 4.5 per 1,000 detected by mammography alone. The recall rate was 3.5 percent in both groups. DBT alone detected 72 of 80 cancers found in the DBT and digital mammography group.
“Tomosynthesis and digital mammography is much more sensitive than digital mammography,” said the study’s principal investigator, Pierpaolo Pattacini, MD, radiologist and director of the radiology department at AUSL Reggio Emilia in Reggio Emilia, Italy. “The vast majority of the advantage is due to tomosynthesis alone.”
While DBT’s higher sensitivity would seem to make it a logical choice for breast cancer screening programs, more research is needed to weigh the benefits against any undesired effects. The gain in detection for combined digital mammography and DBT was higher for ductal carcinoma in situ than for invasive cancer. Among invasive cancers, the gain in detection was similar for both cancers smaller than 10 mm and cancers between 10 and 20 mm, while there was no gain in the detection for larger cancers.
“If these small cancers never became life-threatening, then we are increasing overdiagnosis and not impacting mortality,” said coauthor Paolo Giorgi Rossi, PhD, director of the epidemiology unit at AUSL Reggio Emilia. “Thus, we need to have a measure of the impact of this higher detection rate on the incidence of advanced cancers and interval cancers in the following years.”
The additional reading time DBT would require is another consideration. According to the researchers, implementing tomosynthesis in public screening programs would require rethinking protocols and reading technologies to reduce or eliminate the extra costs.
The new research represents a preliminary analysis from the Reggio Emilia Tomosynthesis trial (RETomo), a larger study in which researchers will be looking at interval cancers and cumulative incidence of advanced cancers. To have more precise and reliable estimates of these outcomes, the researchers are promoting a network of ongoing trials on tomosynthesis with similar study design across Europe.
“Once we have this evidence, the consequences for screening could be even larger than a simple shift from digital mammography to tomosynthesis,” Dr. Giorgi Rossi said. “For example, it could be appropriate to adopt longer intervals between screenings.”
Web Extras
- Access the study, “Digital Mammography versus Digital Mammography Plus Tomosynthesis for Breast Cancer Screening: The Reggio Emilia Tomosynthesis Randomized Trial,” at https://pubs.rsna.org/doi/full/10.1148/radiol.2018172119