Cost Effectiveness Colorectal Screenings
New research shows that CT colonography is a less-invasive screening with less-extensive preparation and lower risk of complications than colonoscopy.
BY MELISSA SILVERBERG
October 01, 2018

Stoker

Lansdorp-Vogelaar
Nevertheless, data using actual screening results to compare the cost-effectiveness of CT colonography and colonoscopy screening has been lacking, said researcher Jaap Stoker, MD, chair of the Division of Radiology & Nuclear Medicine, Radiotherapy and Rehabilitation Medicine at the University of Amsterdam.
“Until now, research on the cost effectiveness of CT colonography in colorectal cancer screening was based on assumptions,” Dr. Stoker said. “This, to our knowledge, is the first study to use actual screening results.”
In a recent Radiology study, Dr. Stoker and colleagues used screening results in the Netherlands to examine the cost-effectiveness of two colorectal cancer screening modalities: colonoscopy and CT colonography screening.
The Netherlands — like most of Europe — screens for colorectal cancer on a nationwide basis.
Dr. Stoker has been part of a research group examining colorectal cancer screening in the Netherlands for several years.
Another author on the study, Iris Lansdorp-Vogelaar, MD, associate professor at the Department of Public Health of Erasmus Medical Center (MC) in Rotterdam, is part of a research group at the institution that was one of the first to develop a population-based decision model to evaluate the cost-effectiveness of cancer screening. The Erasmus MC group urged the Dutch government to introduce an organized colorectal cancer screening program in the country.
As part of that conversation, decision makers at a consensus meeting in 2004 sought to determine which test was optimal to implement nationwide. Pilot studies began in several areas: fecal occult blood testing, fecal immunochemical testing and sigmoidoscopy, CT colonography and colonoscopy.
Although colonoscopy is considered the gold standard, researchers noted that perceived burden of preparation for the test, cost and other drawbacks can deter patients from participating. Comparatively, CT colonography is a less-invasive screening with less-extensive preparation and lower risk of complications.
In 2012, a large randomized controlled trial in the Netherlands (the Colonoscopy or Colonography for Screening [COCOS] trial) was the first to compare the participation, yield and unit costs of CT colonography and colonoscopy in a dedicated screening setting.
“Until now, research on the cost effectiveness of CT colonography in colorectal cancer screening was based on assumptions,” Dr. Stoker said. “This, to our knowledge, is the first study to use actual screening results.”
In a recent Radiology study, Dr. Stoker and colleagues used screening results in the Netherlands to examine the cost-effectiveness of two colorectal cancer screening modalities: colonoscopy and CT colonography screening.
The Netherlands — like most of Europe — screens for colorectal cancer on a nationwide basis.
Dr. Stoker has been part of a research group examining colorectal cancer screening in the Netherlands for several years.
Another author on the study, Iris Lansdorp-Vogelaar, MD, associate professor at the Department of Public Health of Erasmus Medical Center (MC) in Rotterdam, is part of a research group at the institution that was one of the first to develop a population-based decision model to evaluate the cost-effectiveness of cancer screening. The Erasmus MC group urged the Dutch government to introduce an organized colorectal cancer screening program in the country.
As part of that conversation, decision makers at a consensus meeting in 2004 sought to determine which test was optimal to implement nationwide. Pilot studies began in several areas: fecal occult blood testing, fecal immunochemical testing and sigmoidoscopy, CT colonography and colonoscopy.
Although colonoscopy is considered the gold standard, researchers noted that perceived burden of preparation for the test, cost and other drawbacks can deter patients from participating. Comparatively, CT colonography is a less-invasive screening with less-extensive preparation and lower risk of complications.
In 2012, a large randomized controlled trial in the Netherlands (the Colonoscopy or Colonography for Screening [COCOS] trial) was the first to compare the participation, yield and unit costs of CT colonography and colonoscopy in a dedicated screening setting.
CT Colonography Deemed More Cost-Effective
In the Radiology study, researchers used data from the COCOS trial to simulate situations with the Dutch population aged 25-85 using different CT colonography and colonoscopy screening scenarios. The participation rates for colonoscopy and CT colonography were 21.5 percent (1,276 of 5,924 invitees) and 33.6 percent (982 of 2920 invitees), respectively.
The model was used to predict colorectal cancer incidence and mortality, cost of screening and life years gained by screening for each scenario. Researchers were then able to determine an optimal screening strategy based on cost-effectiveness analysis.
Because of the 56 percent higher participation rates, CT colonography was determined to be more cost-effective than colonoscopy screening, results showed. Yet results were different when factoring equal attendance.
“We found that with equal attendance, colonoscopy is more cost-effective than CT colonography,” Lansdorp-Vogelaar said. “However, because the pilot study (COCOS) found significantly higher attendance for CT colonography compared to colonoscopy, CT colonography was more cost-effective than colonoscopy in that situation.”
In the Radiology study, researchers used data from the COCOS trial to simulate situations with the Dutch population aged 25-85 using different CT colonography and colonoscopy screening scenarios. The participation rates for colonoscopy and CT colonography were 21.5 percent (1,276 of 5,924 invitees) and 33.6 percent (982 of 2920 invitees), respectively.
The model was used to predict colorectal cancer incidence and mortality, cost of screening and life years gained by screening for each scenario. Researchers were then able to determine an optimal screening strategy based on cost-effectiveness analysis.
Because of the 56 percent higher participation rates, CT colonography was determined to be more cost-effective than colonoscopy screening, results showed. Yet results were different when factoring equal attendance.
“We found that with equal attendance, colonoscopy is more cost-effective than CT colonography,” Lansdorp-Vogelaar said. “However, because the pilot study (COCOS) found significantly higher attendance for CT colonography compared to colonoscopy, CT colonography was more cost-effective than colonoscopy in that situation.”
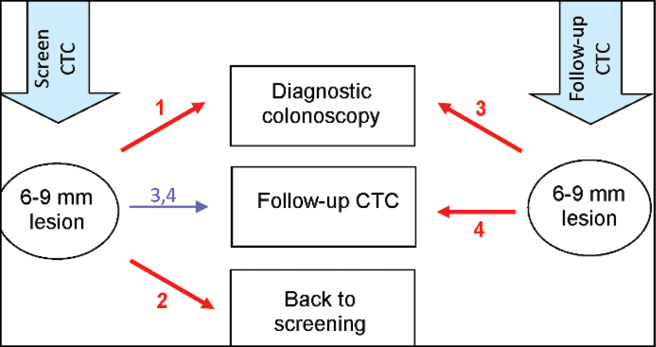
Diagram shows the four simulated follow-up strategies for CT colonography (CTC ) screening that differ when 6–9-mm adenomas are found. In all four strategies, individuals with lesions of at least 10 mm at CT colonography were immediately referred for diagnostic colonoscopy, and individuals without lesions or with lesions measuring 1–5 mm at CT colonography returned to the screening program. Follow-up strategies differed in management of medium-sized lesions (6–9 mm) seen at CT colonography. Individuals with medium-sized lesions (1) were directly referred for diagnostic colonoscopy (ie, by using a cutoff of 6 mm); (2) were returned to screening program (ie, corresponding with a 10-mm cutoff); (3, 4) were offered follow-up CT colonography after 3 years, as was done in the Colonoscopy or Colonography for Screening trial, and referred to diagnostic colonoscopy if they at follow-up CT colonography had a medium or large lesion (3) or a large lesion (4). In the 4th strategy, persons with medium-sized adenomas continued to receive follow-up CT colonography, either until a large lesion was detected or until a medium lesion was no longer detected. van der Meulen, M. et al., Radiology 2018:287;3 © RSNA 2018
Results Have Wide-Ranging Impact
Results showed that the cost-effectiveness of CT colonography is most applicable in a national screening program offering a single test modality, which is the case in most programs.
And while the study was conducted in the Netherlands, researchers say the results are relevant for other populations.
“Although absolute participation rates and costs may differ among countries, the relative differences between CT colonography and colonoscopy primarily determine the comparative effectiveness,” Dr. Stoker said.
The results could aid health care decision makers as they consider introducing screening methods and also serve as an important reminder for countries that do not offer nationwide cancer screening programs.
“I hope that clinicians and policy makers realize that the best test may not necessarily be the test with the best performance characteristics,” Dr. Lansdorp-Vogelaar said. “Although colonoscopy is superior to CT colonography in detecting neoplasia, because fewer people accept it, on a population level it actually does not perform as well.”
Results showed that the cost-effectiveness of CT colonography is most applicable in a national screening program offering a single test modality, which is the case in most programs.
And while the study was conducted in the Netherlands, researchers say the results are relevant for other populations.
“Although absolute participation rates and costs may differ among countries, the relative differences between CT colonography and colonoscopy primarily determine the comparative effectiveness,” Dr. Stoker said.
The results could aid health care decision makers as they consider introducing screening methods and also serve as an important reminder for countries that do not offer nationwide cancer screening programs.
“I hope that clinicians and policy makers realize that the best test may not necessarily be the test with the best performance characteristics,” Dr. Lansdorp-Vogelaar said. “Although colonoscopy is superior to CT colonography in detecting neoplasia, because fewer people accept it, on a population level it actually does not perform as well.”
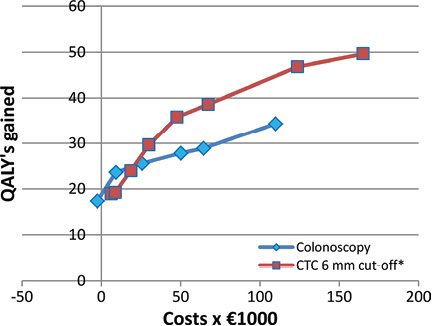
Graph shows modeled costs and quality-adjusted life-years (QALYs) gained per 1,000 invitees of CT colonography (CTC) strategies with 6-mm cutoff and colonoscopy with different starting and stopping ages and screening intervals, with 3 percent discounting, from a population’s perspective. * = CT colonography strategy as described in the diagram on page 15. van der Meulen, M., et al., Radiology 2018:287;3 © RSNA 2018
Colorectal Imaging Focus of RSNA 2018 Sessions
Imaging of the Colorectum,” will be presented on Tuesday, Nov. 27, from 4:30 to 6:30 p.m. Sessions include:
- CT Colonography: Technique Update
- CT Colonography: Strategies for Success
- MRI Rectal Cancer Including Structured Reporting
- MRI Anorectal Fistulas Including Structured Reporting
Science Session with Keynote: Gastrointestinal (Colorectal Imaging),”will be presented on Wednesday, Nov. 28, at 10:30 a.m.
ASRT@RSNA 2018: CT Colonography — The New Kid on the Block,” will be presented on Wednesday, Nov. 28, from 2:20 to 3:20 p.m.
Select a datasource