Knee Arthritis Made Worse with Steroid Injections
Popular treatment can lead to weakened cartilage, increased risk of damage and accelerated osteoarthritis

Researchers comparing two injections commonly used to relieve knee pain from osteoarthritis—corticosteroid and hyaluronic acid—found that corticosteroid injections were associated with higher progression of the disease. The research was published in Radiology.
Hyaluronic acid was associated with decreased progression on MRI up to two years post-injection.
According to the World Health Organization (WHO), osteoarthritis affects about 528 million people worldwide. With a prevalence of 365 million, the knee is the most frequently affected joint, according to the WHO. Many patients with knee osteoarthritis seek non-invasive treatment for pain relief through corticosteroid or hyaluronic acid injections.
“Our study directly challenges a common clinical practice: the use of corticosteroid injections for knee osteoarthritis symptom relief,” said Upasana Upadhyay Bharadwaj, MD, who was a research fellow in the Department of Radiology at University of California, San Francisco, at the time of the research. “It presents robust evidence that corticosteroids accelerate structural knee degeneration, even after a single injection.”
For the study, researchers evaluated the association between intra-articular injections and osteoarthritis progression using a whole-organ semi-quantitative MRI evaluation (WORMS) and clinical outcomes over a two-year period.
Data was analyzed from 210 participants from the Osteoarthritis Initiative, a multicenter, longitudinal, observational study of nearly 5,000 men and women with knee arthritis—sponsored by the National Institutes of Health—currently in its 14th year of follow-up.
The research team looked at 70 participants who had one injection in the knee—either corticosteroid or hyaluronic acid—and who had knee MRIs taken before, at the time of, and two years after the injection.
They used WORMS to assess how much damage had occurred in different parts of the knee joint over time. These scores were compared to a control group of 140 individuals with similar characteristics who did not receive any injection.
“This study is the first to use WORMS to assess the progression of knee osteoarthritis following a single intra-articular injection of either corticosteroids or hyaluronic acid, with a two-year follow-up,” Dr. Upadhyay Bharadwaj said. “Prior studies relied predominantly on X-ray assessments or advanced quantitative MRI requiring specialized postprocessing. Unlike those, this study uses semi-quantitative scoring feasible in clinical settings and isolates patients who received only one injection.”
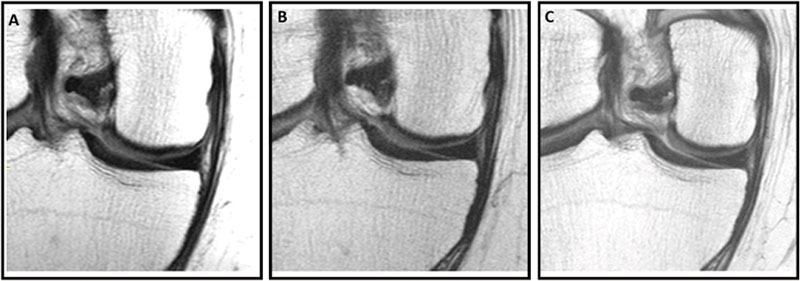
Knee MRI scans in a 57-year-old male participant in the Osteoarthritis Initiative who was administered a hyaluronic acid (HA) injection. Coronal intermediate-weighted knee MRI scans obtained (A) 2 years before injection, (B) at the time of injection, and (C) 2 years after injection show a well-preserved medial femoral cartilage, indicating a stable medial femoral cartilage through the pre- and postinjection time points. The medial femoral cartilage appears well-preserved across all three time points, suggesting no structural deterioration following the HA injection. These findings indicate stable cartilage morphologic structure during the 4-year observation period.
https://doi.org/10.1148/radiol.233081 ©RSNA 2025
More Cautious Use Recommended
Of the 70 patients who received injections, 44 were injected with corticosteroids and 26 were injected with hyaluronic acid. The treatment and control groups were matched by age, sex, body mass index, pain and physical activity scores, and severity of disease.
The study found that corticosteroid injections led to more knee joint damage over the two-year period than both the control group and those who received hyaluronic acid injections, Dr. Upadhyay Bharadwaj noted.
In contrast, hyaluronic acid injections were linked to less progression of joint damage and even appeared to slow down the damage compared to before the injection. Both types of injections helped reduce knee pain, but only hyaluronic acid seemed to help without causing further joint harm.
“The most striking finding is that a single corticosteroid injection led to significantly greater structural damage in the knee joint over two years, especially in cartilage, while hyaluronic acid injections not only avoided this damage but actually showed reduced joint deterioration post-injection,” she said. “Corticosteroids are known to reduce inflammation but also impair the repair mechanisms of cartilage and can inhibit matrix synthesis.”
Over time, this may lead to weakened cartilage and increased susceptibility to damage, accelerating the progression of osteoarthritis.
“There is also evidence of subchondral bone changes and risk of insufficiency fractures linked to steroid injections,” Dr. Upadhyay Bharadwaj said. “This study could lead to more judicious use of corticosteroid injections, especially for patients with mild to moderate osteoarthritis who are not yet surgical candidates.”
Dr. Upadhyay Bharadwaj said that clinicians may opt for hyaluronic acid injections more frequently or consider alternative pain management strategies that don't accelerate structural deterioration. Guidelines might evolve to recommend against routine use of corticosteroids in favor of approaches with better long-term safety profiles for joint health.
“Given their widespread use, these findings could influence clinical guidelines and patient care decisions, encouraging more cautious use and stronger consideration of alternatives like hyaluronic acid,” she said. “The public impact is significant, as osteoarthritis is a major global cause of disability, and millions receive such injections annually.”
For More Information
Access the Radiology article, “Intra-articular Knee Injections and Progression of Knee Osteoarthritis: Data from the Osteoarthritis Initiative.”
Read previous RSNA News stories on musculoskeletal imaging:
- High-Quality Symptom Information Dramatically Improves the Reports of Lumbar Spine MRI
- Capturing the Body in Motion: How 4D CT Acquires Dynamic Imaging of the Musculoskeletal System
- How AI Is Reshaping Musculoskeletal Imaging