Intravascular Ultrasound Catheters Let Interventional Radiologists Get Creative
Common and emerging uses refine the practice of IR


In concert with the RadioGraphics monograph, RSNA News recognizes the contributions of interventional radiology in patient care. Find additional research and articles at RSNA.org/News and RSNA.org/RadioGraphics.
As devices for vascular imaging get sleeker and smarter, interventional radiologists are applying imaginative techniques to evaluate and treat a new spectrum of conditions.
“Interventional radiologists are problem solvers by nature,” said Eric Monroe, MD, associate professor in pediatric radiology and vascular & interventional radiology at the University of Wisconsin in Madison. “Creative solutions and novel applications help us to solve challenging clinical questions— and that improves patient care and outcomes.”
Advances in intravenous ultrasound (IVUS) catheters have opened more possibilities. While single-element, slower- emitting catheters produced images that were often contaminated by electronic noise and wedge-shaped defects in the field of vision, the newer generation allows concentric placement over a guidewire channel with less rigidity, reduced noise and high frequencies, producing crisp circular images across a wide range of diameters.
A CME-eligible article co-authored by Dr. Monroe and colleagues in RadioGraphics describes how these devices can be applied in a variety of novel situations.
Complementary and Expanded Interventions Support Standard of Care
• Venous interventions
IVUS offers high-detail images of acute venous conditions such as thrombosis or inflammatory vein wall thickening, as well as of chronic disease like thrombosis, stenosis, valvular dysfunction, fibrosis, or intravascular spurs. In patients with compressive syndromes, the technique can optimize targeted interventions.
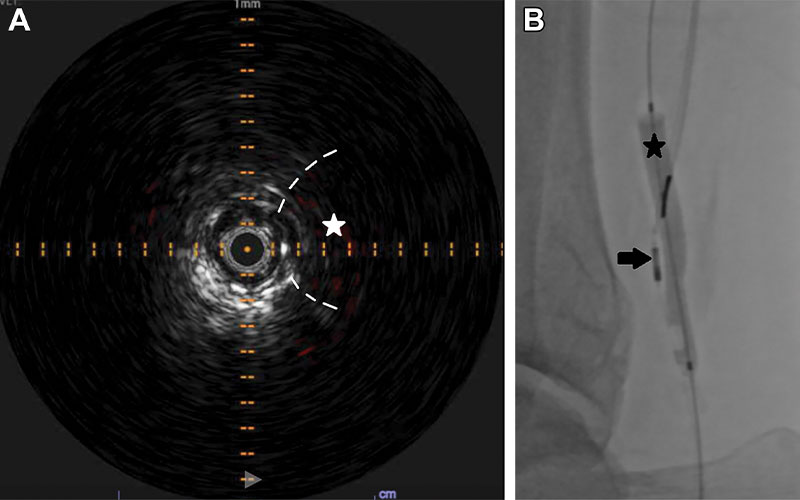
• May-Thurner syndrome
While venography can depict extrinsic compression and collateral outflow, adding IVUS may reveal chronic vessel wall changes and luminal abnormalities such as bridging fibrotic spurs, helping to solidify a May-Thurner syndrome diagnosis. After the decision to place a stent, IVUS can add more confidence to sizing and deployment. The authors caution against selecting stents based on patient sex or weight.
“We have a variety of techniques for stent sizing, but the addition of ultrasound allows us to directly assess the area to be treated,” said co-author Erica Knavel Koepsel, MD, assistant professor in interventional radiology at the University of Wisconsin. Additional co-authors of the study include, Jeffrey Forris Beecham Chick, MD, MPH, University of Washington, and Michael A. Woods, MD, University of Wisconsin. “Rather than a ‘one size fits all’ approach, we can proceed with improved accuracy and a tailored method of patient care,” Dr. Knavel Koepsel said.
https://doi.org/10.1148/rg.220015 ©️RSNA 2022
• Nutcracker syndrome
Stent placement is a promising alternative to surgery for patients with this condition, but the rate of stent migration is concerning, the authors wrote. As with iliac vein stent planning, IVUS can add complementary morphologic information for patients being considered for renal auto transplantation.
• Chronic venous thrombosis
IVUS can help confirm appropriate intraluminal access through an occluded segment. Sonographic information on thrombus chronicity can inform selection of appropriate interventional devices—and avoid those interventions that may be unhelpful. IVUS also can better characterize stenoses and guide stent size selection.
• IVC filter placement
For patients who are can’t be moved or for those who are too heavy for the angiography table, IVUS-guided placement of IVC filters is an established choice.
• Portal venous interventions
Creating a transjugular intrahepatic portosystemic shunt (TIPS) by using fluoroscopy alone can be tricky because of anatomical variants. In 20%-30% of patients, variants occur in the course and number of hepatic veins and portal veins and up to half of patients have an extrahepatic portal vein bifurcation, the authors explained. Incorporating side-firing IVUS guidance can help to reduce access attempts, capsular perforations, procedure time, and radiation dose.
• Arterial interventions
IVUS has long been the reference standard for in vivo coronary vessel wall imaging, outperforming angiography for disease characterization. “For similar reasons, uses in aortic and peripheral arterial applications have increased along the way,” the authors write. Rather than infer pathology from the planar appearance of the opacified vascular lumen, IVUS provides direct visualization, making way for applications in both atherosclerotic and nonatherosclerotic disease of the arterial tunicae, as well as extrinsic compressive lesions such as in popliteal entrapment syndrome.
• Peripheral vascular disease and atherosclerosis
“Compared with arteriography alone, IVUS more accurately defines the true arterial dimensions, plaque type (soft, fibrous, calcified or mixed), plaque morphology (length, shape, volume and concentric verses eccentric), and associated disorders such as dissection or thrombosis,” the authors note.
• Aortic disorders
IVUS can complement pre- and intraprocedural imaging for stent-graft treatment of thoracic or abdominal aortic aneurysms. IVUS has led to more precise endograft placement while reducing early endoleaks, contrast agent use and intraprocedural radiation.
• Intravascular and transvenous biopsy
When intravascular or otherwise difficult-to-access lesions are in close proximity to large veins, IVUS can significantly improve accuracy, the authors said, following with a series of illustrated tips for successful biopsy.
Future Directions May Change Diagnosis and Treatment Landscape
The authors predict that not only will interventional radiologists continue to modify established technology in innovative ways, but the technology itself will continue to evolve to fit the applications.
“Ultrasound is a fantastic diagnostic and interventional modality,” Dr. Knavel Koepsel said. “Expanding its use has helped us become more precise and controlled in our interventions and has also enabled visualization of anatomy and pathology in a brand-new way.”
For More Information
Access the RadioGraphics article, “Intravascular US: Applications in Interventional Radiology."
Read previous RSNA News stories on interventional radiology:
- The Growing Popularity of IR/DR Certification
- Minimally Invasive Fistula Creation A Promising Option For Dialysis Patients
- The Effect of COVID-19 on Interventional Radiology Around the Globe