Advances in Fetal Imaging Show Promise for Prenatal and Postnatal Care
Emerging prenatal imaging markers aid in differential diagnosis of congenital lung malformations and suprarenal lesions



As prenatal imaging has grown increasingly sophisticated at lesion identification, diagnostic certainty has remained a challenge. Two recent studies characterize prenatal imaging markers for differential diagnosis of lung and suprarenal lesions. These markers may help in prenatal diagnosis and postnatal treatment planning.
The Hyperintense Bronchus Sign
Differential diagnosis of congenital lung malformations in the prenatal stage remains difficult due to a paucity of clear imaging marker descriptions. However, an imaging marker indicative of airway obstruction may help diagnose congenital lung malformations prenatally with high accuracy.
In a Radiology study published in May, researchers found that an MR imaging characteristic called the hyperintense bronchus sign (HBS) is a marker of a blocked airway and is observed with more prevalence in certain congenital lung malformations.
“In our analysis of lung lesions in prenatal MRI scans, we identified a linear T2 hyperintensity within the lungs,” said co-author Gregor Kasprian, MD, associate professor of radiology in the Department of Biomedical Imaging and Image-Guided Therapy at the Medical University of Vienna. “We call this the hyperintense bronchus sign.”
“Our findings indicate that the HBS is caused by airway obstruction, and we can use it to distinguish, with a high sensitivity, among lesions such as bronchial atresia and sequestration, and CCAM,” said lead author Florian Prayer, MD, who is also a PhD student at the Medical University of Vienna.
Drs. Prayer and Kasprian and their team evaluated a data set consisting of 248 prenatal lung MRI studies of 177 babies with congenital lung malformations, including postnatal diagnostic CT scans and histopathological analyses. The 16-year retrospective study in collaboration with Texas Children’s Edward B. Singleton Department of Radiology allowed them to determine the prevalence of the HBS in different lung lesions.
Watch Drs. Kasprian and Prayer discuss their research into the hyperintense bronchus sign:
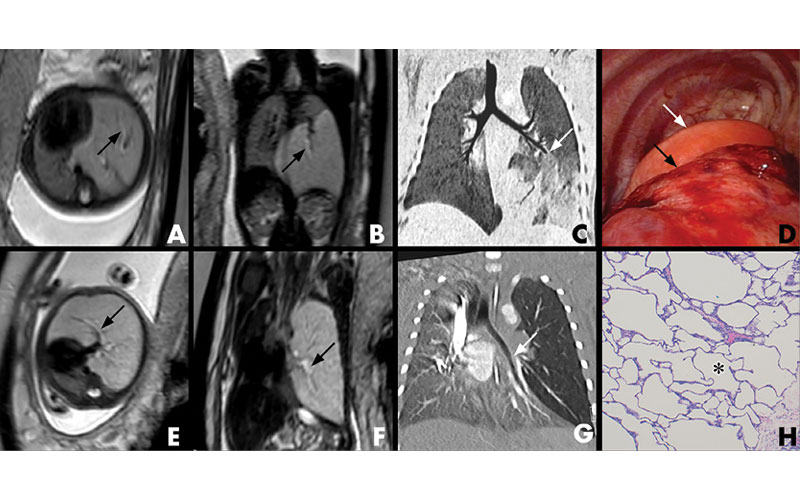
The HBS was most prevalent in cases of bronchial atresia (BA), followed by bronchopulmonary sequestration (BPS), and was most visible up to 26 gestational weeks.
“We found the HBS in almost 80% of BA cases and in 70% of BPS cases,” Dr. Prayer said. “This can help to distinguish BA and BPS from other lung lesions, not only early in pregnancies but also non-invasively.”
Early diagnosis of congenital lung lesions buys time for families to plan for postnatal treatment and allows clinicians to more confidently advise either surgery or monitoring.
The detection of the HBS may also reduce the need for postnatal imaging.
“Utilizing the HBS in prenatal diagnosis could also mitigate later radiation by avoiding excessive postnatal CT follow-ups,” Dr. Kasprian said.
Differential Diagnosis of Suprarenal Lesions
Although prenatal suprarenal lesions are uncommon, their diagnostic challenge lies in their diverse pathologies, treatments and outcomes.
In a retrospective multicenter review of suprarenal lesions diagnosed in 44 babies using prenatal US and MRI, unique imaging characteristics between pulmonary sequestrations and adrenal hemorrhages emerged. The review was published by Fetal Diagnosis and Therapy in April.
“In our study of prenatal US and MRI, the most common suprarenal lesion diagnoses were subphragmatic extralobar pulmonary sequestration and adrenal hemorrhage,” said co-author Danielle Richman, MD, staff radiologist at Brigham and Women’s Hospital of Harvard Medical School in Boston.
“Through statistical analysis of their imaging appearance, we identified markers for differential diagnosis.”
Pulmonary sequestrations were universally left-sided and more likely to appear solid on US, Dr. Richman explained. They also featured a feeding vessel on US or MRI, had a low T1 MRI signal, and did not contain blood products. Conversely, adrenal hemorrhages could appear on both sides and were more likely to have a cystic component. Adrenal hemorrhages did not contain a feeding vessel, and typically demonstrated T1 MRI signal, indicating the presence of blood products.
"Our study provides additional information to allow the health care provider to more confidently diagnose prenatally detected suprarenal lesions. This will help healthcare providers counsel parents about the expected follow-up and outcome.”
DANIELLE RICHMAN, MD
Notably, the majority of prenatal suprarenal lesions in this study were benign, and spontaneously regressed either pre- or postnatally. A smaller percentage of lesions that persisted underwent treatment or surgery, indicating an overall patient benefit of early detection.
These distinct prenatal imaging characteristics, which differentiate between subdiaphragmatic pulmonary sequestration and adrenal hemorrhages as well as the observation of regression patterns, have diagnostic and treatment implications.
“Our study provides additional information to allow the health care provider to more confidently diagnose prenatally detected suprarenal lesions,” Dr. Richman said. “This will help health care providers counsel parents about the expected follow-up and outcome.”
Promising Findings Require Further Research
Both studies provide promising prenatal diagnostic imaging markers, but researchers also emphasize the need for continued research.
Dr. Richman and her colleagues acknowledge that the small sample size of their study didn’t allow for comparative analysis of other suprarenal lesions, such as upper quadrant cysts and neuroblastoma. This may be an area of further study.
Drs. Prayer and Kasprian note that while the HBS marker has potential, the question of whether or not to operate on a congenital lung lesion remains unsolved.
“Some lesions can become malignant and require surgery, others may cause chronic inflammation and infection; however, the more we improve in determining the nature of those lesions prenatally, the better we can help prospective parents prepare for the postnatal care,” Dr. Prayer said.
For More Information
Access the Radiology study, “Characterization of the Hyperintense Bronchus Sign as a Fetal MRI Marker of Airway Obstruction.”
Access the Fetal Diagnosis and Therapy study, “Prenatal Imaging Diagnosis of Suprarenal Lesions,” at Karger.com.
Read previous RSNA News articles on pediatric imaging: