AI Improves Breast Cancer Risk Prediction
Deep neural network proves more accurate than density-based models

A sophisticated type of artificial intelligence (AI) can outperform existing models at predicting which women are at future risk of breast cancer, according to a study published in Radiology.
Most existing breast cancer screening programs are based on mammography at similar time intervals — typically, annually or every two years—for all women. This “one size fits all” approach is not optimized for cancer detection on an individual level and may hamper the effectiveness of screening programs.
“Risk prediction is an important building block of an individually adapted screening policy,” said study lead author Karin Dembrower, MD, breast radiologist and PhD candidate from the Karolinska Institute in Stockholm, Sweden. “Effective risk prediction can improve attendance and confidence in screening programs.”
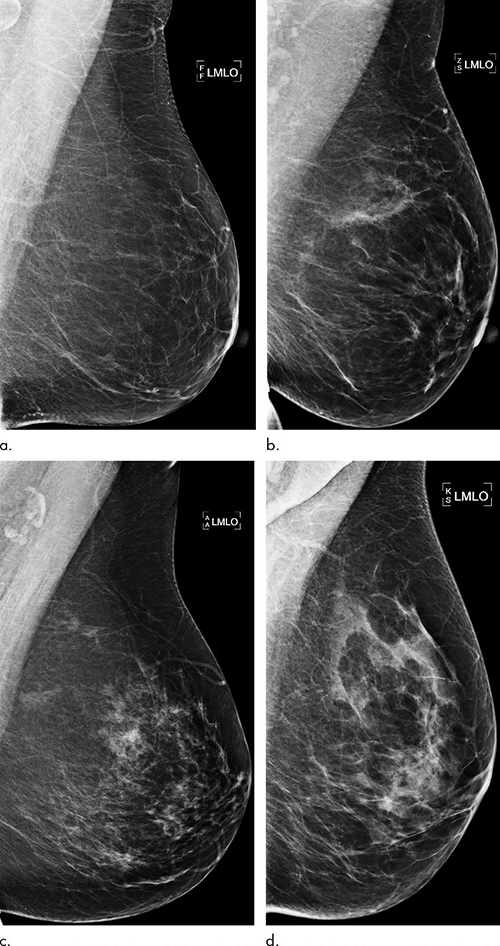
While high breast density may be incorporated into risk assessment, current prediction models may fail to fully take advantage of all the rich information found in mammograms. This information has the potential to identify women who would benefit from additional screening with MRI.
Dr. Dembrower and colleagues developed and trained a deep neural network risk model on mammograms from cases diagnosed between 2008 and 2012 and then studied on more than 2,000 women ages 40 to 74 who had undergone mammography in the Karolinska University Hospital system. Of the 2,283 women in the study, 278 were later diagnosed with breast cancer.
The deep neural network showed a higher risk association for breast cancer compared to the best mammographic density model (odds ratio: 1.6 and 1.3, respectively). The false-negative rate was lower for the deep neural network than for the best mammographic density model (31% vs. 36%; P = .006). The difference was most pronounced for women later diagnosed with more aggressive cancers.
AI Model Can be Improved
The study findings support a future role for AI in breast cancer risk assessment.
“We are not reporting mammographic density currently,” Dr. Dembrower said. “In the introduction of individually adapted screening, we use deep learning networks trained to predict cancer rather than taking the indirect route that density offers.”
As an additional benefit, the AI approach can continually be improved with exposure to more high-quality data sets.
“Our deep learning experts at the Royal Institute of Technology in Stockholm are working on an update to the model,” Dr. Dembrower said. “After that, we aim to test the model clinically next year by offering MRI to the women who stand to benefit the most.”
For More Information
Access the study, "Comparison of a Deep Learning Risk Score and Standard Mammographic Density Score for Breast Cancer Risk Prediction."