Iron Measurements with MRI Reveal Stroke’s Impact on Brain
MRI R2* mapping may have a role in monitoring patient’s recovery from stroke.
March 12, 2019
Tourdias
A simple MRI method that measures iron content can provide a more comprehensive picture of the consequences of stroke-related damage to the brain, according to a study published in Radiology.
Strokes can result in significant impairments caused by infarction and long-term outcomes may be affected by delayed degeneration of brain areas away from the location of the stroke. One such area is the substantia nigra (SN).
“Overall, the SN is strongly involved in motor control, but also in regulation of emotions, cognition and motivation,” said study co-author Thomas Tourdias, MD, PhD, professor of radiology at the Centre Hospitalier Universitaire in Bordeaux, France. “Usually, stroke doesn’t directly affect the SN but, by interrupting circuits, stroke can induce secondary degeneration of that area.”
Prior to the new study, this secondary degeneration of SN had only been seen on post-mortem brain examinations. Imaging on a living person has not been able to capture the long-term degeneration, so for the new study, Dr. Tourdias and colleagues employed MRI R2* mapping to measure iron content in the brain.
Research Finds Iron Content Associated with Poorer Outcomes
The researchers used MRI R2* mapping to evaluate 181 patients who had suffered a stroke. One year after a baseline evaluation, some of the patients showed higher iron content in the SN. This high iron content was associated with worse long-term outcomes, particularly when it was found on the same side of the brain that the stroke occurred.
“We showed that imaging of iron can also be used to image degeneration remotely from stroke in disconnected areas,” Dr. Tourdias said. “This finding could be clinically useful because it shows that a simple magnetic resonance imaging method such as R2* can provide a more comprehensive picture of the consequences of an infarct.”
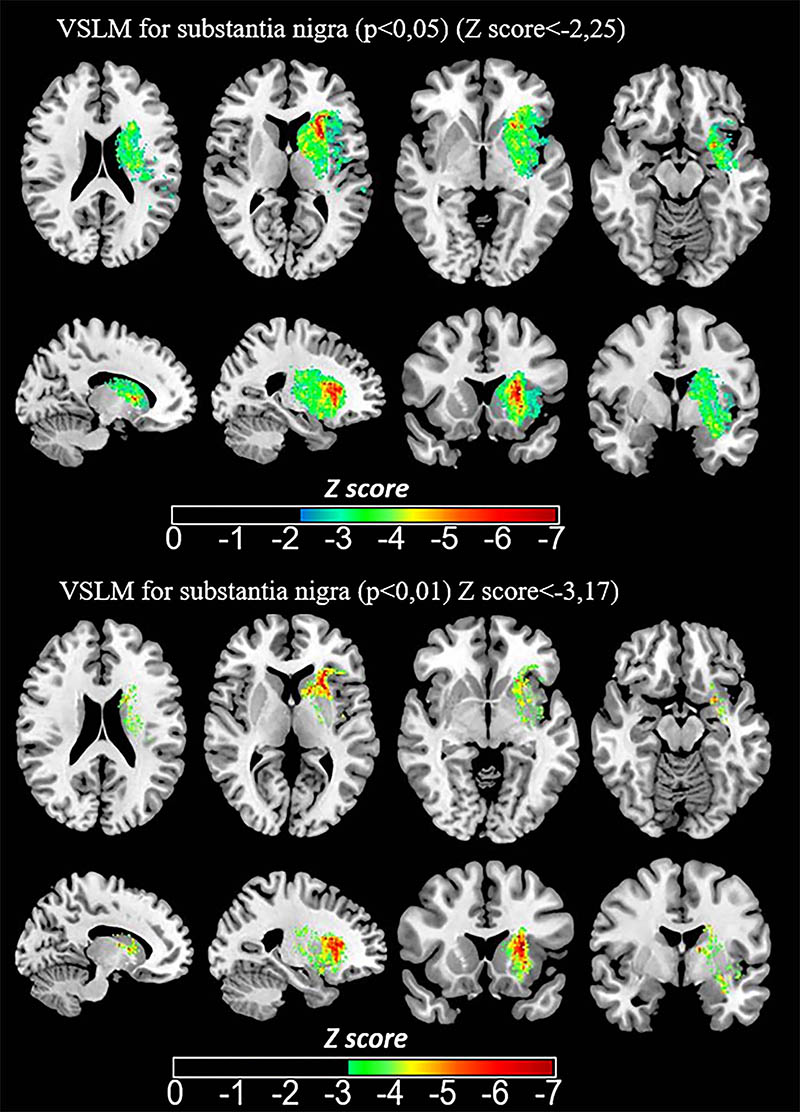
Images show voxel-based lesion-symptom mapping (VLSM) quantified impact of baseline infarct location on SN-AI95 of R2∗ at 1-year follow-up. Z score resulting from Brunner-Menzel testing is indicated by color range and is overlaid on three-dimensional T1-weighted image normalized to Montreal Neurological Institute 152 space atlas in axial, sagittal, and coronal planes. Association between infarct voxels and higher SN-AI95 is shown by lower Z score.
The results suggest that R2* mapping may be added to the follow-up MRI after stroke to monitor neurodegeneration, Dr. Tourdias said, by assessing iron levels in the SN. More generally, the findings lend support to the use of iron imaging as a marker for neurodegeneration, an idea that is already being explored for neurodegenerative diseases like Parkinson’s disease. Therapies that prevent iron deposition could potentially be used to slow or stop the degeneration of the neurons.
“We are currently investigating this direction,” Dr. Tourdias said. “Our imaging approach could become crucial in the clinic if modulation of iron develops as a neuroprotective strategy in the future.”
Access the Radiology study, “Neurodegeneration of the Substantia Nigra after Ipsilateral Infarct: MRI R2* Mapping and Relationship to Clinical Outcome,” at pubs.radiology.org.