Synthetic Imaging: Novel Methods of Image Creation Bring Benefits
Benefits include reducing radiation dose, scan time and cost without compromising outcomes


As imaging technology continues to evolve, radiologists are exploring how synthetic imaging can help reduce the amount of time patients spend getting scans and lower the amount of radiation they are exposed to, while still making a proper diagnosis.
Synthetic imaging is a simulation method which allows reconstruction of multiple image contrasts, with different photographic densities, from one scan. This can be done in two different methods.
In the first, the synthetic (simulated) images are generated from parametric maps of tissue properties after MR acquisition. The maps contain measured parameters for each voxel, which allow virtual scanner metrics that correspond to those used in conventional scans, such as echo time, repetition time and inversion time.
The second method uses deep learning to take the data from one imaging modality and use it to generate data that replicates another modality or uses deep learning to improve the quality of scans that might be of lower quality. For example, an MR scan can be used to create analogous CT images without the patient having been in a CT scanner.
Synthetic Imaging Offers Lower Radiation Dose in Mammography
In mammography, synthetic imaging can help reduce the amount of radiation patients are exposed to, said Samantha Zuckerman, MD, MBE assistant professor of clinical radiology (breast imaging) at the University of Pennsylvania, Philadelphia.
In 2011, the FDA approved Digital Breast Tomosynthesis (DBT) for use in breast cancer screening and diagnosis along with digital mammography as a way to improve cancer detection rates and lower the rates of recalling women for additional screenings. However, the change has resulted in doubling the amount of radiation women are exposed to compared with screening via mammography alone.
A study published in Radiology by Dr. Zuckerman and her colleagues assessed whether replacing digital mammography with a combination of DBT and a non-radiation alternative like synthetic imaging could produce the same results.
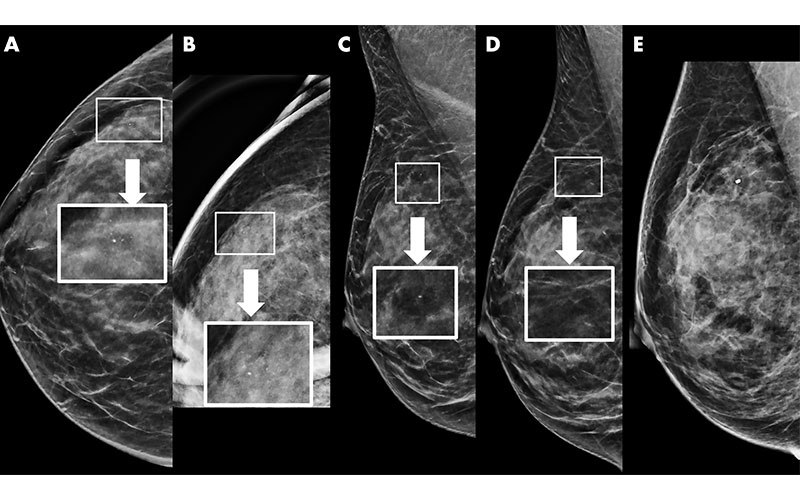
Example of synthetic imaging calcification enhancement in a 43-year-old woman who presented for screening. A, Screening mammogram obtained with synthetic imaging (craniocaudal view). New faint amorphous calcifications are seen in the outer breast. Finding was classified as Breast Imaging Reporting and Data System (BI-RADS) category 0. Inset image was obtained at ×3 magnification. B, Diagnostic mammogram, two-dimensional magnification view (craniocaudal view), confirms the presence of calcifications; however, they are of equal or less conspicuity compared with that seen with synthetic imaging. Inset image was obtained at ×3 magnification. Finding was classified as BI-RADS category 4. C, Screening mammogram obtained with synthetic imaging (mediolateral oblique view). New faint amorphous calcifications are seen in the superior breast. They are less conspicuous compared with those on the craniocaudal view in A. Finding was classified as BI-RADS category 0. Inset image was obtained at ×3 magnification. D, Diagnostic digital mammogram obtained at recall (mediolateral view). Calcifications are much less conspicuous on two-dimensional digital mediolateral view. Inset image was obtained at ×3 magnification. Finding was classified as BI-RADS category 4. E, Diagnostic mammogram obtained with two-dimensional imaging after biopsy (digital mediolateral view). The clip is in appropriate location. Pathologic examination showed ductal carcinoma in situ, intermediate grade.
https://doi.org/10.1148/radiol.2020200240 ©RSNA 2022
According to the authors, synthetic mammography (SM) was developed to decrease the radiation dose to women undergoing DBT. SM is not meant to be an exact replica of digital mammography. The reconstruction algorithm purposefully enhances areas, such as calcifications and potential areas of architectural distortion, to make them more conspicuous to the radiologist.
The research team conducted a retrospective study of more than 150,000 screening examinations from the University of Pennsylvania and the University of Vermont between 2011 and 2018. They found no statistically significant difference in biopsy rate, false-negative rate, cancer detection rate or other outcomes for women who underwent SM/DBT versus those who underwent DBT and digital mammography. This demonstrated that breast cancer screening performance can be maintained within benchmarks when synthetic mammography replaces digital mammography in digital breast tomosynthesis imaging.
“I am excited about synthetic imaging because it preserves the benefits of tomosynthesis imaging while decreasing the radiation dose to patients,” Dr. Zuckerman said.
Now, all screening examinations at the University of Pennsylvania are done using SM/DBT rather than digital mammography.
“In the future, I hope to help educate other centers about how to best interpret synthetic imaging so that they too can replace their digital mammography screening study with synthetic imaging,” she said.
Benefits Of Using Deep Learning to Enhance Imaging Quality
A Magnetic Resonance Image Compilation (MAGiC) trial demonstrated that synthetic MRI provided similar quality to that of conventional proton-density, STIR, and T1- and T2-weighted contrast views across neurologic conditions. While the MAGiC trial revealed challenges with the synthetic T2 FLAIR images, these were readily recognizable and did not mimic pathology.
To date, the primary benefit of synthetic MR imaging is in segmentation and quantitation e.g of brain myelin, said Suzie Bash, MD, medical director of neuroradiology at San Fernando Valley Interventional Radiology at RADNET.
Despite early promise for reduced brain acquisition times with synthetic MRI, the greatest potential for imaging speed with synthetic MRI is likely to be found elsewhere within the body, perhaps for spine and MSK evaluations when conventional acquisitions of multiple different contrasts in the same imaging plane are typically scanned and conventional acceleration opportunities are less robust.
AI-based-tools, such as deep learning, are having a significant impact throughout the imaging enterprise, by improving image quality while reducing acquisition times.
In a multi-reader, multicenter, prospective trial published by the American Journal of Neuroradiology, Dr. Bash and her colleagues found that deep learning provided 60% faster scan times while maintaining high volumetric quantification accuracy, consistent clinical classification, and what radiologists perceive as superior image quality across all imaging features, when compared with standard of care.
"Interestingly, deep learning can also be leveraged to overcome image quality shortcomings of synthetic FLAIR T2 once available for synthetic sequences," Dr. Bash said.
Decreasing image acquisition time has significant patient-centric benefits.
According to Dr. Bash, 30% of patients experience significant anxiety or claustrophobia during a traditional MRI. A shorter scan can also reduce the likelihood of motion artifact which degrades image quality. Dr. Bash noted that over a quarter of inpatient or emergency department scans need to be repeated either partially or completely due to movement, which is costly and time consuming for both patients and health care institutions.
For More Information
Access the Radiology study, “Multicenter Evaluation of Breast Cancer Screening with Digital Breast Tomosynthesis in Combination with Synthetic versus Digital Mammography' and the accompanying editorial, "Mounting Evidence for Synthetic Mammography in Breast Cancer Screening."
Access the American Journal of Neuroradiology study at ajnr.org.
Read previous RSNA News articles about synthetic imaging