Screening Mammography Could Benefit Men at High Risk of Breast Cancer
Landmark 12-year study shows personal history of breast cancer a significant risk factor

Selective mammography screening can provide potentially lifesaving early detection of breast cancer in men who are at high risk for the disease, according to a landmark study published in the journal Radiology.
Breast cancer in men is a rare but often deadly disease. The American Cancer Society projects that 2,670 new cases of invasive breast cancer will be diagnosed in men in 2019, and about 500 men will die from it.
In the first study of its kind, lead author Yiming Gao, M.D., from the Department of Radiology at New York University Langone Medical Center in New York City, and colleagues evaluated the pattern of male breast imaging utilization to determine high-risk screening outcomes and to delineate risk factors associated with cancer diagnosis.
There are no formal screening guidelines for men in high-risk groups such as those who have a personal history of the disease, breast-cancer-associated genetic mutations or family members who had breast cancer. As a result, men diagnosed with breast cancer tend to have worse outcomes than women. For the retrospective study, researchers used the screening mammography benchmarks in women based on the fifth edition of American College of Radiology BI-RADS definitions to assess outcomes in the screening group.
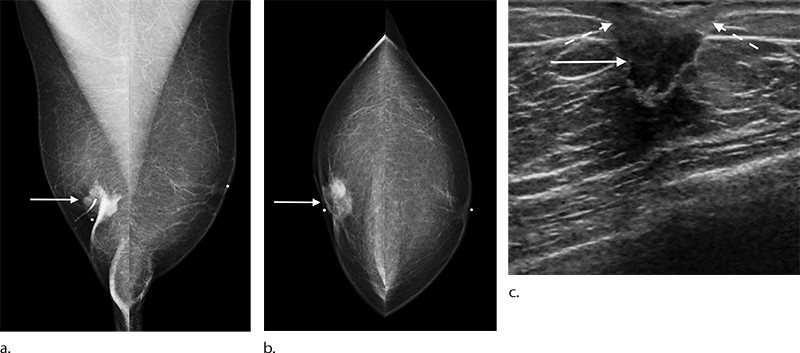
Researchers evaluated breast imaging utilization patterns and screening outcomes in 1,869 men, median age 55, who underwent mammography over a 12-year period. During the study period, mammograms were obtained by using full-field digital mammography (between 2005–2016) or digital breast tomosynthesis (between 2016–2017). Ultrasound was performed by using 7–12-MHz linear array transducers (between 2005–2006) and 14-MHz transducers (between 2006–2017).
All men undergoing screening had personal or family history of breast cancer and/or genetic mutations.
Potential For Early Disease Detection
Mammography helped detect a total of 2,304 breast lesions, 149 of which were biopsied. Of those, 41 (27.5 %) proved to be malignant. The cancer detection rate of 18 per 1,000 exams in men at high risk of breast cancer was significantly higher than the average detection rate of three to five per 1,000 exams in average risk women. In addition, the cancers in men detected were at an early stage, before they had spread to the lymph nodes, improving the prognosis for survival.
“These results show that it is possible to detect male breast cancer early, and it appears that mammography is effective in targeted screening of high-risk men,” Dr. Gao said. “We’ve shown that male breast cancer doesn’t have to be diagnosed only when symptomatic.”
In men, the study showed that mammographic screening sensitivity was 100 percent, while specificity was 95 percent, which researchers say is related to men having a relative lack of breast fibroglandular tissue that in women often masks abnormal results.
Personal history of breast cancer was the most significant risk factor associated with breast cancer in men. Ashkenazi Jewish ancestry, genetic mutations, and first-degree family history of breast cancer were also significant factors. This potential for early disease detection in men is supported by the fact that 90% of male breast cancers are ductal in origin and up to 98% of precursors to invasive male breast cancers are ductal carcinoma in situ, typically seen as calcifications at mammography.
Currently, the National Comprehensive Cancer Network (NCCN) does not support screening because of a lack of evidence, even in men with elevated risk. Earlier NCCN guidelines suggested consideration of baseline mammograms on an individual basis, an approach the new study results may support.
Moving forward, the researchers hope to see larger multi-institutional studies that have the statistical power to delineate more nuanced information based on different breast cancer risk factors in men.
“Rethinking our strategy toward male breast cancer diagnosis is necessary,” Dr. Gao said. “We hope these results will provide a foundation for further investigations, and potentially help pave the way to standardizing screening for certain high-risk groups of men.”
For More Information
Access the Radiology study, “Breast Cancer Screening in High-Risk Men: A 12-Year Longitudinal Observational Study of Male Breast Imaging Utilization and Outcomes."