International Radiology Consensus Outlines Best Practices for Post-COVID CT
Global team of experts hope to standardize chest CT use in patients recovering from post-COVID pneumonia

Experts representing multiple societies and institutions across 14 countries have published guidance for computed tomography (CT) imaging in patients with residual lung abnormalities after COVID-19 illness. The consensus statement appears in Radiology.
The statement’s authors seek to standardize the indications for when chest CT is appropriate for patients with post–COVID-19 condition, the methods for acquiring images and the terminology used for reporting residual lung abnormalities. The final consensus was reviewed by four expert pulmonologists to ensure alignment with clinical perspectives.
Using standardized and specific terminology when reporting these abnormalities helps to avoid confusion with interstitial lung diseases (ILDs), explained statement coauthor Anna Rita Larici, MD, an associate professor of radiology at Catholic University of the Sacred Heart of Rome and chief of the Chest Imaging Unit at Advanced Radiology Center of Agostino Gemelli University Polyclinic Foundation in Rome. It also helps physicians make more informed decisions about patient management, and it captures more precise data for future research.
“These statements recommend employing terms from the Fleischner Society Glossary to describe CT findings consistently and precisely, avoiding the use of ‘interstitial lung abnormality (ILA),’ which refers to a different clinical context,” Dr. Larici said. “In addition, we have coined and recommended the term ‘post–COVID-19 residual lung abnormality’ to prevent any misleading term when describing CT lung abnormalities following COVID-19 pneumonia.”
The authors also outlined the conditions under which chest CT imaging is appropriate for this patient group. They recommend chest CT for patients whose respiratory symptoms continue or worsen three months after infection, with these symptoms lasting for at least two months and with no other explanation. A chest CT scan three to six months after discharge may also be considered for all patients hospitalized with moderate to severe COVID-19 due to the high rate of residual CT lung abnormalities observed in these patients.
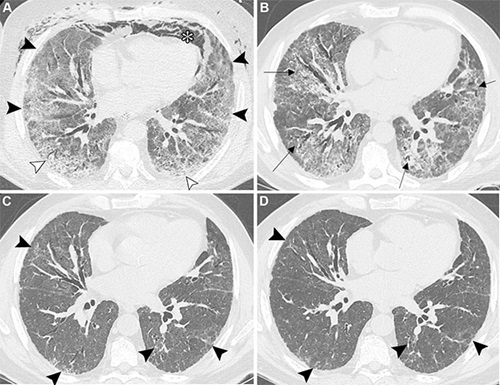
Unenhanced axial CT images show post–COVID-19 residual abnormalities in a 69-year-old male patient with a history of smoking and myocardial infarction. (A) Baseline image obtained at admission to intensive care department shows extensive ground-glass opacities and mild bilateral consolidation (black arrowheads), associated with crazy paving pattern (white arrowheads), spontaneous pneumomediastinum (*), and bilateral anterior chest wall subcutaneous emphysema. (B) Image obtained 1 month later shows complete resolution of the pneumomediastinum and subcutaneous emphysema, with persistent diffuse bilateral ground-glass opacities and reticular opacities. Mild lung and bronchial architectural distortion are also observed (arrows). The patient was discharged with instructions to use supplemental oxygen during exertion and at night. (C) Image obtained 4 months from baseline shows the reduction of prior ground-glass opacities and reticular opacities, with residual patchy areas of mild ground-glass opacities and fine reticular opacities showing subpleural and peribronchovascular distribution (arrowheads) in both lungs. Previously observed bronchial dilation shows improvement. The patient reported persistent mild exertional dyspnea, and pulmonary function tests revealed a mild restrictive pattern and slightly reduced diffusing lung capacity for carbon monoxide. (D) Image obtained at 1-year follow-up shows near-complete resolution of post–COVID-19 lung abnormalities, with only minimal residual ground-glass opacities and mild architectural distortion (arrowheads).
https://doi.org/10.1148/radiol.243374 © RSNA 2025
Adherence to Low-Dose Protocol is Critical
The group suggests that follow-up be guided by radiological expertise in conjunction with clinical judgment, considering its frequency based on the extent of initial lung abnormalities, temporal changes and/or pulmonary physiology.
Radiologists should adhere to the “as low as reasonably achievable” (ALARA) principle for serial CT follow-up, using a low-dose protocol within a range of 1 to 3 millisieverts, the authors advised.
“Radiologists play a crucial role in adhering to ALARA principles by optimizing CT protocols—using appropriate low-dose techniques during follow-ups—while maintaining the image quality necessary for accurate assessment,” Dr. Larici said. “This is especially important when serial imaging of these patients is needed, so that we minimize radiation exposure without compromising diagnostic accuracy.”
COVID-19 can cause continuing or worsening symptoms after infection—described as post–COVID-19 condition or “long COVID”—and approximately 6% of individuals who have had COVID-19 are estimated to experience post–COVID-19 condition. Among patients hospitalized for acute COVID-19, on average, 50% show chest CT abnormalities, and 25% have restrictive pulmonary functional abnormalities at four months after infection. Radiologists face several unique challenges when caring for this patient population.
“These include differentiating between persistent residual COVID-19 lung abnormalities and evolving fibrotic changes, interpreting overlapping features such as ground-glass opacities versus fibrosis, and assessing the temporal evolution of these findings,” Dr. Larici explained. “Distinguishing post–COVID-19 residual lung abnormalities from ILA and ILDs is crucial, because they have very different clinical implications: post–COVID-19 changes typically stabilize over time, whereas ILA and ILDs can progress.”
It’s important to understand that post–COVID-19 lung abnormalities can persist for months and potentially impact respiratory health, she said.
“Follow-up imaging plays a key role in assessing these residual changes and guiding clinical care, but it should be performed judiciously. Adherence to established recommendations helps ensure that patients receive follow-up imaging and care only when clinically indicated,” Dr. Larici said.
Dr. Larici noted that being part of a global team of experts working together signifies a collective effort to establish evidence-based, harmonized best practices for caring for patients recovering from post–COVID-19 pneumonia.
“It reflects a commitment to advancing patient care worldwide through shared knowledge, research and consensus,” she said.
For More Information
Access the Radiology article, “Best Practice: International Multisociety Consensus Statement for Post–COVID-19 Residual Abnormalities on Chest CT Scans,” and the related editorial, “Post-COVID-19 Chest CT Expert Consensus, and a Nod to the Law of the Instrument.”
Read previous RSNA News stories on COVID-19: