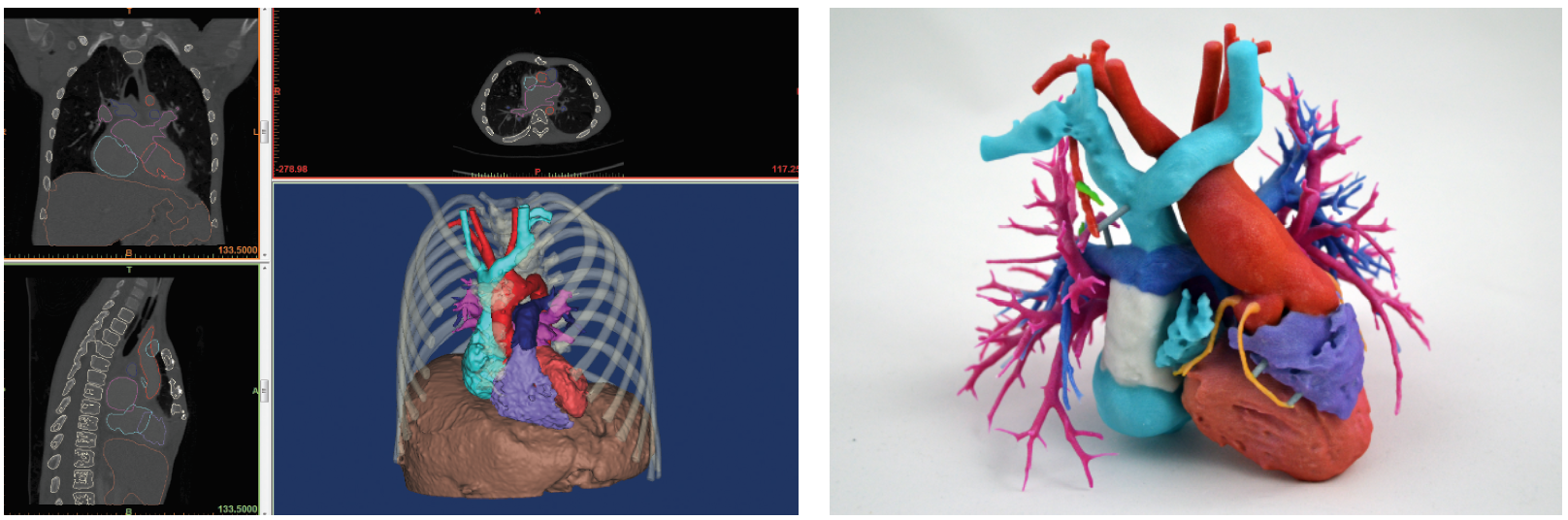
3D Printed Models Add Colorful New Dimension to Complex Surgery
3D printed models are aiding surgeons performing complex surgery
Editor’s Note:This is the third in a three-part series on the 3D printing explosion in radiology. Read parts one and two.
Just a few days after her daughter Jemma’s birth, Stephanie Starks found herself living a nightmare. Jemma had dangerously low levels of oxygen in her blood and had been rushed to Phoenix Children’s Hospital, where doctors discovered a life-threatening congenital defect in her heart. As doctors prepared for emergency surgery, Stephanie was frightened and confused.
One doctor told her Jemma had been born with only half a heart; another said she had “pulmonary atresia with intact ventricular septum.” None of it made any sense, not even when a cardiologist tried to draw Stephanie a picture of her daughter’s heart on a sheet of paper.

Suddenly, the cloud lifted, and for the first time since she had arrived at the hospital, Stephanie felt reassured.
“At first, heart surgery is this unknown that you can’t picture, like the scary monster under the bed,” she recalled. “But when they show the 3D model, it takes away so much of the fear. It changes everything.”
Doctors agree that the 3D model offers a valuable new tool to relay the complexity of surgery to patients.
Jemma is now four years old and thriving, and Stephanie has become what she calls a “volunteer cheerleader” for 3-D printing. The Starks have two 3-D models of Jemma’s heart on the mantle above their fireplace and Stephanie wears a miniaturized model of the heart on a necklace that is a way of “keeping my daughter’s heart close to mine,” she said.
Collaboration Critical to 3D Printing
Jemma’s case and others like it are further evidence that 3D printing for medicine has arrived in a big way. Models are used in a growing number of applications across different specialties. Early adopters, like Frank Rybicki, MD, Jonathan Morris, MD, and Jane Matsumoto, MD, are senior leaders and central figures in the RSNA’s 3D Printing Special Interest Group (SIG), helping to pave the way for younger SIG members like Dr. Ryan. The RSNA 3D Printing SIG was launched in November 2016.

Cutting Guides Chart Surgical Course


RSNA 3-D Printing Special Interest Group Leads the Way
The combination of increasing demand and falling prices for models is likely to accelerate the growth of 3-D printing, Dr. Rybicki said, creating challenges for radiology leaders working to establish practice standards and ensure that the highest quality models are used for appropriate applications — ideas that the RSNA SIG has focused on since its inception.
“The SIG has had wonderful feedback and support from the RSNA senior leadership, and we are planning to disseminate our initial recommendations document,” he said. “It remains important for the SIG to provide stewardship in best practices for medical 3-D printing as enthusiasm and importance in the field continues to grow.”
Once standards and a framework of appropriateness are established, reimbursement can enter the discussion, according to Dr. Rybicki. While the sentiment building around 3-D printing is important, Dr. Rybicki emphasized that data will ultimately move the needle on reimbursement. A key upcoming study is 3-D Hearts Enabling a Randomized Trial, or 3-DHEART, a multi-site clinical trial of 400 pediatric congenital heart patients in which Dr. Ryan is a primary investigator.
With the support of the 3-D printing companies Stratasys and 3D Systems, researchers will analyze the impact of 3-D printed hearts based on MRI or CT scans of young patients. The primary focus of the two-year study is to see if the 3-D models reduce the need for cardiopulmonary bypass surgery.
“We’re very excited to see what the results will be on bypass rates,” Dr. Ryan said. “We will also be capturing 24 secondary metrics, like time in and time out, morbidity and readmission rates."
Important advances lie ahead and collaboration will be central to transforming technology into better and more efficient patient care.
“Our emerging leaders will be those who can best understand and communicate this, and the senior leaders today will have to provide the mentorship to nurture and guide the great level of enthusiasm for the field,” Dr. Rybicki said.
