Smoking Impedes Embolization Treatment in Lungs
Inflammatory response caused by smoking creates greater likelihood of PAVM failure
Smoking reduces the chances of a successful procedure to treat blood vessel abnormalities in the lungs, according to a study in Radiology.
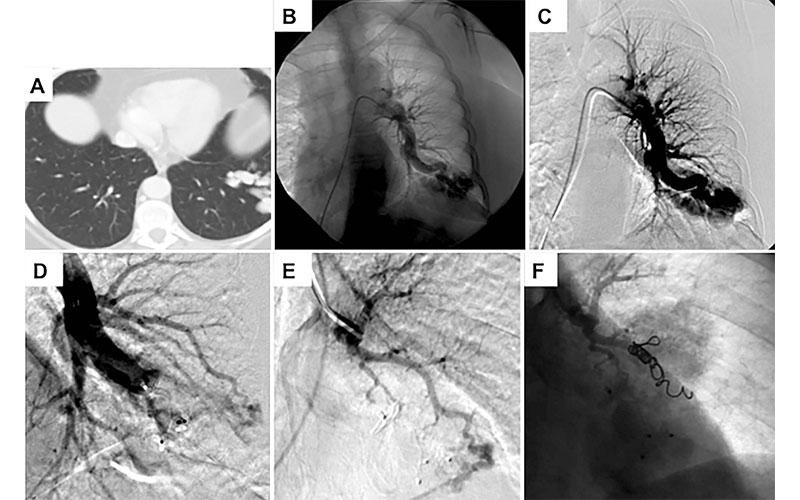
Pulmonary arteriovenous malformations (PAVMs) are abnormal connections between arteries and veins in the lungs. The abnormalities can become symptomatic and lead to potentially dangerous complications. PAVMs are strongly associated with an inherited disorder called Hereditary Hemorrhagic Telangiectasia (HHT).
“HHT is a disease that can manifest with patients having AVMs in their lungs,” said study senior author Sanjay Misra, MD, an interventional radiologist at the Mayo Clinic Department of Radiology in Rochester, MN. “When these AVMs become symptomatic, we are asked to embolize them using coils.”
In the embolization procedure, a catheter is threaded from a large blood vessel in the leg to the site of the PAVM. A small coil is then inserted to block the PAVM. The procedure is highly effective, but the PAVMs will persist in some patients.
Long-term Smokers Face Higher Levels of PAVM Recurrence
For the new study, Dr. Misra and colleagues wanted to see how smoking might affect post-embolization PAVM persistence rates. They looked at 103 patients with HHT who underwent embolization for a total of 373 PAVMs. The patients were classified into smoking or non-smoking groups.
Smokers faced a higher rate of PAVM persistence following treatment than those who had never smoked. Patients reporting active tobacco use at the time of PAVM embolization had a five-year persistence rate of 26.3% compared with 13.5% in inactive smokers.
PAVMs persisted after treatment in more than a third of smokers with more than 20 pack-years, compared with only 12.2% of nonsmokers. Pack years is a measure of smoking intensity that accounts for how long and how much a person has smoked.
“Our five-year data showed that the cumulative incidence of persistence was 17.3%, or almost one in five patients,” Dr. Misra said. “Smoking more than 20 pack years was associated with a fivefold increase in PAVM recurrence.”
While the study did not assess the reason for the post-embolization persistence of PAVMs in smokers, previous research has linked smoking with inflammation and abnormalities in the formation of new blood vessels.
“Smoking creates an inflammatory response,” Dr. Misra said. “More inflammation creates a greater likelihood of failure for smokers compared to those who never smoked.”
The findings, if confirmed in larger studies, could be used to advise patients with HHT who might be considering embolization for PAVMs.
“Smoking cessation is very important if these patients want to help themselves and avoid further procedures,” Dr. Misra said. “We should urge current smokers to stop smoking before treatment.”
For More Information
Access the full Radiology study and results at, “Smoking Significantly ImpactsPersistence Rates in Embolized Pulmonary Arteriovenous Malformations inPatients with Hereditary Hemorrhagic Telangiectasia," and read the accompanying editorial, "Persistence of Pulmonary Arteriovenous Malformation after Embolization: Another Reason to Quit Smoking."