Radiology Review Reports on the State of Vaping Associated Lung Injury
Researchers say rapidly evolving public health care crisis could be the tip of the iceberg

With research and understanding of electronic cigarettes or vaping associated lung injury (EVALI) still evolving, a new Radiology review looks at the current state of the disease, diagnostics and the need for continued research.
Published online, “Radiologic, Pathologic, Clinical, and Physiologic Findings of Electronic Cigarette or Vaping Product Use–associated Lung Injury (EVALI): Evolving Knowledge and Remaining Questions,” is the newest research to tackle EVALI, a rapidly evolving public health crisis that has led to more than 2,500 hospitalizations since August, according to the Centers for Disease Control (CDC).
As of January, the CDC had reported more than 2,600 cases of EVALI reported from 50 states, the District of Columbia and two U.S. territories (Puerto Rico and U.S. Virgin Islands), and 60 deaths reported from 27 states and the District of Columbia. All reported cases have a history of e-cigarette product use or vaping.
Recent research shows that most EVALI patients have smoked e-cigarettes that contained some mixture of marijuana and nicotine products, but study authors Seth Kligerman, MD, and Mark Schiebler, MD, say part of the problem is lack of regulation of vape pens and their contents.
In cases of EVALI reported to the CDC, 86% reported using products containing either nicotine or THC. The lack of regulation, black-market vape products and a young demographic of users all make researching the issue more complicated. The dramatic increase in vaping among middle school and high school students over the past year represents the largest increase in use of any illicit substance tracked by the National Institute of Drug Abuse over the last 44 years, according to the review.
“It all boils down to what is it that they are smoking? What they tell you they are smoking is not necessarily what they have been smoking. We have no idea what’s in these cartridges and sometimes they don’t know either, so there is a lot that’s unknown,” said Dr. Schiebler, professor of radiology at the University of Wisconsin School of Medicine and Public Health, Madison.
Other variabilities including the amount a patient inhales each time, length of inhalation, the volume of substance inside the vape pen and frequency of vaping can all make this research more challenging, said Dr. Kligerman, chief of cardiothoracic imaging and associate professor of radiology at UC San Diego Health.
Scratching the Surface of EVALI
Both doctors said that while the cases of EVALI seem to have slowed down after reaching a peak last fall, there is still much doctors don’t know about acute and long-term effects.
“We’re scratching the surface of this disease,” Dr. Schiebler said. “I worry that vape pens are delivering particles to the lungs that we’ve never seen before in volumes we’ve never seen before. We are watching long-lasting lung and vascular injury happening before our eyes and this could be the tip of the iceberg.”
“Right now we are just talking about acute lung injury, but I think this is going to be relatively minor in relation to the chronic injuries we’re going to see if people continue to vape in the numbers they are,” Dr. Kligerman added. “We just don’t know what the chronic effects are yet.”
Originally touted as an alternative to traditional cigarettes, e-cigarettes still contain nicotine and have been marketed primarily to young adults with brightly colored packaging, advertising and flavoring.
Dr. Schiebler said the next phases of research will include epidemiology to trace particular outbreaks back to types of e-cigarettes and their contents, pathology to collect and study cases of EVALI and look for patterns, and research into particle size and how it affects the lungs over time.
“At this juncture, what we do not know far exceeds what we do know, and numerous questions remain unanswered,” the authors write.
Dr. Kligerman said radiologists still have an important role to play in looking for lung injury patterns consistent with possible EVALI and asking doctors to ask about vaping when they are talking with patients.
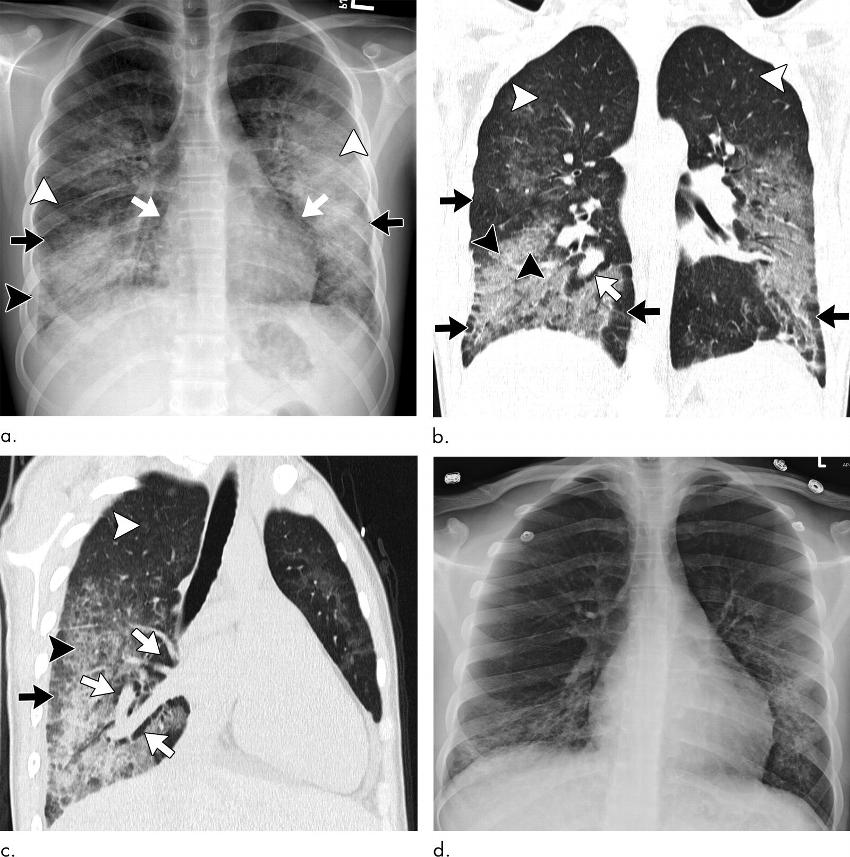
The study reports that in most cases, both the imaging and pathologic findings of EVALI are that of organizing pneumonia and diffuse alveolar damage, although the disease can appear differently on scans for some people.
“There are findings that the rapid initiation of supportive care and in some cases the use of corticosteroids can help improve patient outcomes or lessen the severity of the injury,” Dr. Kligerman said.
Because EVALI is such a new condition and vaping is a rapidly growing patient behavior, it is not yet a part of most electronic medical records. Dr. Schiebler says that needs to change so that physicians are reminded to talk to their patients about vaping and track symptoms when they exist.
For More Information
Access the study, "Radiologic, Pathologic, Clinical, and Physiologic Findings of Electronic Cigarette or Vaping Product Use–associated Lung Injury (EVALI): Evolving Knowledge and Remaining Questions."
View the Vaping by the Numbers infographic with stats that detail this health challenge.
Access the Radiology website dedicated to electronic cigarette or vaping product use–associated lung injury (EVALI).
Access information from the Centers for Disease Control and Prevention.