U.S. Clinical Practices Meet or Approach BI-RADS Benchmarks for MRI Breast Screening
Study adds real-world clinical practice data to evidence from clinical trials about breast cancer screening

A new Radiology study comparing data from breast imaging registries throughout the U.S., with Breast Imaging Reporting and Data System (BI-RADS) benchmarks determined that MRI breast screening in community and academic practice meets or approaches current BI-RADS benchmarks.
Lead author Janie M. Lee, MD, MSc, and colleagues compared screening MRI performance in the Breast Cancer Surveillance Consortium (BCSC) with the American College of Radiology’s (ACR) BI-RADS benchmarks. Six regional BCSC registries provided MRI data from 49 facilities across the country.
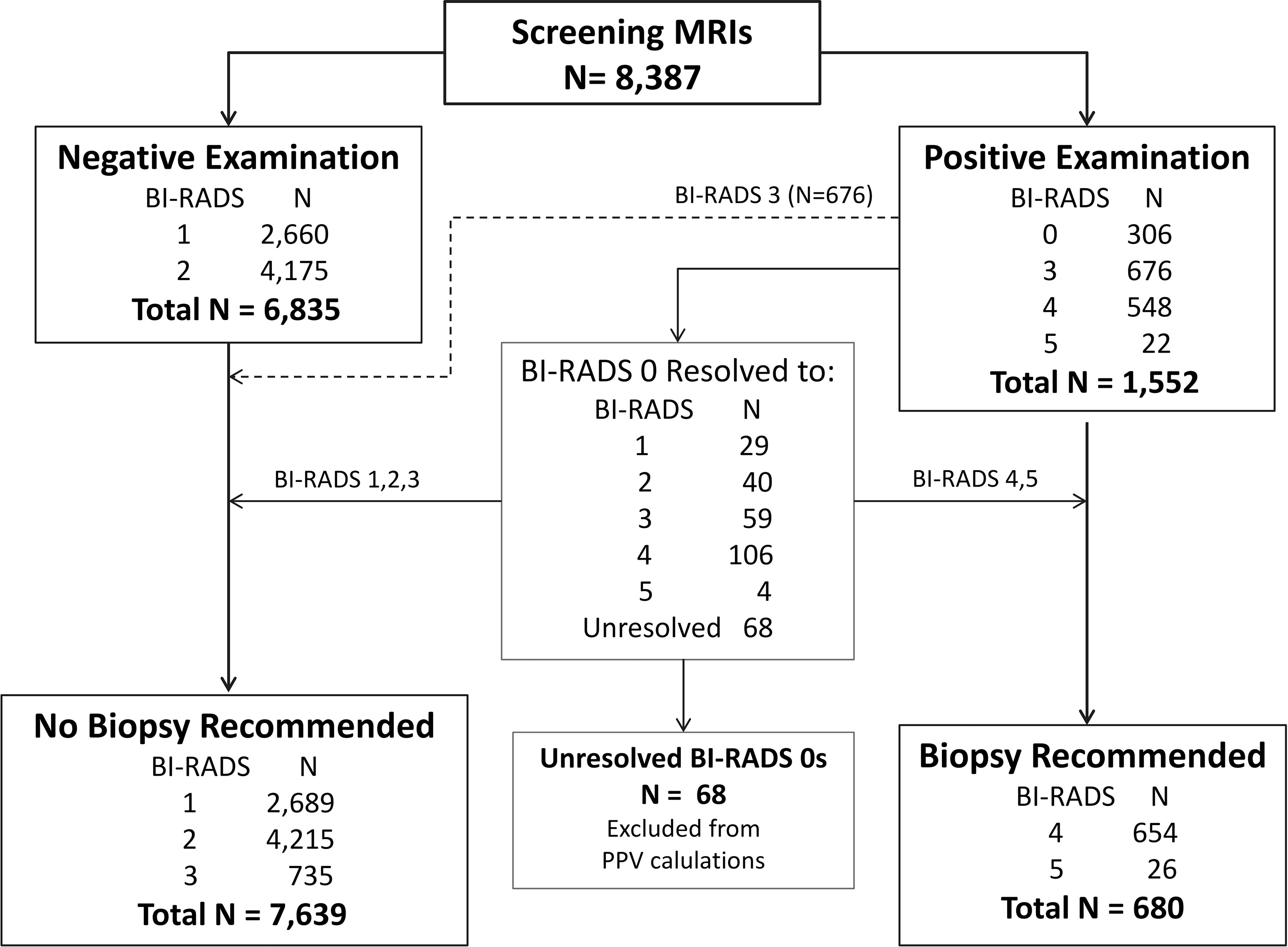
The study examined 8,387 screening breast MRI examinations collected between 2005 and 2013 from 5,343 women. All examinations were linked to state or regional cancer registries to determine if breast cancer was diagnosed within 12 months of an MRI examination.
“Our study looked at community and academic breast imaging facilities, adding data from real-word clinical practice to evidence that we have from clinical trials,” said Dr. Lee, associate professor of radiology at the University of Washington in Seattle and director of breast imaging at Seattle Cancer Care Alliance. “Linking imaging data with breast cancer outcomes gave us the opportunity to examine and calculate all of the performance measures as recommended by the American College of Radiology.”
The Cancer Detection Rate (CDR) observed in the study was 17 per 1,000 screening examinations while the BI-RADS benchmark from clinical trials was 20-to-30 per 1,000 screening examinations.
“This is far higher than five cancers per 1,000, which is the cancer detection rate for mammography in screening women at average risk of breast cancer. These results show that radiologists and referring clinicians are appropriately selecting high-risk women for screening with MRI,” Dr. Lee said.
Practices Encouraged to Compare Benchmarks
MRI specificity, which approached, but did not meet the BI-RADS benchmark of 85-90 percent, suggests that a continued focus on reducing false-positive results remains important in ongoing quality improvement efforts.
The study also provided clinical practice-based values for BI-RADS measures currently noted as “to be determined,” including the percentage of stage 0 or 1 breast cancer diagnosed after screening MRI and the median size of invasive breast cancers. The study determined that 87 percent of breast cancers are detected in stage 0 or 1 and the median size of invasive breast cancer is 10 mm.
“Overall, the results of our study demonstrate that the high performance reported from clinical trials is also achievable in routine clinical practice,” Dr. Lee said. “Our study also contributes additional information which may be used to inform ongoing efforts to update screening MRI performance benchmarks.”
Dr. Lee and colleagues encourage individual practices to compare their performance data with BCSC performance data as well as with BI-RADS benchmarks.
“The continued reporting and collection of clinical practice performance data can help identify areas for quality improvement in breast cancer screening,” Dr. Lee said.
Improving Risk Models also Needed
To support the continued selection of high-risk women for MRI screening, an important area of ongoing study is determining what measure of risk should be used, Dr. Lee said.
“Appropriate selection of high-risk women is important for using imaging technology effectively in screening, and risk communication is an important part of patient selection,” Dr. Lee said.
While the current focus is on lifetime risk of breast cancer, researchers know that this number can change over a woman’s lifetime, Dr. Lee said.
“One important risk communication question is whether shorter-tem risk projections — perhaps over a five-year period — may be more helpful than lifetime risk estimates,” Dr. Lee said. “Further research in this area may help women make better screening decisions.”
Web Extras
- Access the Radiology study, “Performance Benchmarks for Screening Breast MR Imaging in Community Practice,” at http://pubs.rsna.org/doi/abs/10.1148/radiol.2017162033.