Stent Retrievers Improve Odds for Ischemic Stroke Patients

Fast reperfusion leads to improved functional outcome among patients with acute stroke treated with stent retrievers. Detailed attention to workflow with iterative feedback and aggressive time goals may have contributed to efficient workflow environments, according to new research published in the journal, Radiology.
Mayank Goyal, MD, FRCPC, of the University of Calgary in Alberta, Canada, and colleagues analyzed data in the Solitaire with the Intention for Thrombectomy as Primary Endovascular Treatment for Acute Ischemic Stroke (trial SWIFT PRIME). Specifically, researchers examined data in which outcomes were compared in patients treated with intravenous tissue plasminogen activator (tPA) alone or in combination with the Solitaire device.
Researchers determined:
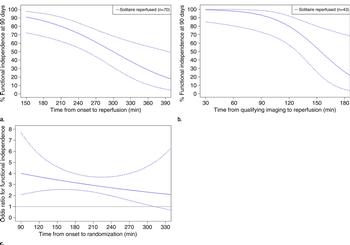
- Revascularization within 2½ hours of symptom onset was associated with functional independence (minimal or no disability) in 91 percent of patients.
- Likelihood of functional independence was 10 percent higher in patients treated within 2½ hours compared with patients treated between 2½ and 3½ hours after stroke onset.
- Every 60-minute delay after 3½ hours resulted in a 20 percent lower likelihood of functional independence.
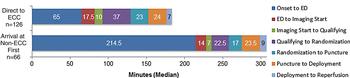
- Upon arrival to the emergency department, sources of delay from imaging acquisition, delivery of patient to the angiography suite, and reperfusion can all be decreased with streamlined workflow.
“Detailed analysis of the workflow in the SWIFT PRIME trial provides further data on the importance of time and efficiency in acute ischemic stroke management, likely contributing to the superior clinical outcome observed in the intervention arm of the trial,” the authors write.
Web Extras
- Access the study, "Analysis of Workflow and Time to Treatment and the Effects on Outcome in Endovascular Treatment of Acute Ischemic Stroke: Results from the SWIFT PRIME Randomized Controlled Trial," at pubs.rsna.org/doi/full/10.1148/radiol.2016160204