MR Neurography an Emerging Modality in Chronic Pain
In a few short years, MR neurography has emerged as a promising inroad into pain diagnosis and management


In a few short years, MR neurography (MRN)—a technique for the direct imaging of spinal and peripheral nerves—is generating excitement as a promising inroad into a perennially challenging area: the diagnosis and management of pain.
In fact, MRN can often be seen as “the poster child for innovation” in the area of musculoskeletal pain and one of the leading developments in that subspecialty over the last four or five years, according to Sandip Biswal, M.D., an associate professor of radiology at the Stanford University Medical Center, who presented “PET and MR Methods to Image Pain” at RSNA 2014.
In America alone, chronic pain affects 116 million adults, resulting in hundreds of billions of dollars annually in treatment costs and lost productivity, Dr. Biswal said. For example, according to a report issued by the Institute of Medicine in 2011, the annual cost of chronic pain in the U.S. is estimated at $560-635 billion—more than the annual costs associated with heart disease, cancer and diabetes combined.
But the “ugly truth,” Dr. Biswal added, is that conventional methods of finding pain generators are just not adequate, which is one of the reasons MRN is generating so much interest.
According to Amelie Lutz, M.D., a colleague of Dr. Biswal who presented the session, “MR Neurography of the Brachial Plexus and Upper Extremities,” with improved scanner and coil techniques, and advances in pulse sequences, “we are now capable of directly imaging nerves with a very high resolution. This has become a really exciting—and evolving—field in radiology.”
What MRN does is “really display the nerves beautifully,” Dr. Biswal said. “We can reconstruct these images in a variety of dimensions and lay out the nerves just as we do with the vascular system. You can really see if there is intrinsic pathology, such as a neuroma or inflammation, or an extrinsic process involving the nerve.”
MRN Breaks Ground with Brachial Plexus
Dr. Lutz discussed the anatomy and normal MR imaging appearance of the brachial plexus and upper extremity nerves and how to recognize the most commonly encountered pathologies and their differential diagnoses in these regions.“With the more central or proximal nerves like the brachial plexus it can be very challenging for nerve conduction studies to really pinpoint or specify the problem. The brachial plexus is probably one of the first areas where this type of imaging is really making an impact,” Dr. Lutz said.
And while the complexity of this anatomic region can appear daunting, she said, with this new tool for systematically analyzing the anatomy, “then all of a sudden it makes sense.”
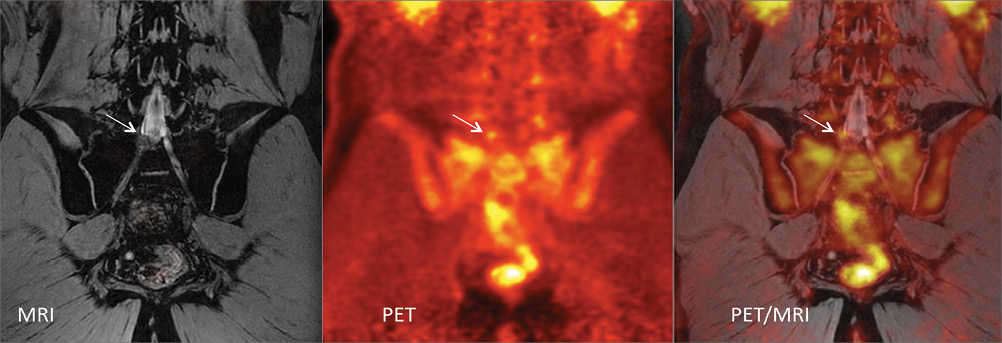
Dr. Biswal discussed a number of new approaches to imaging pain involving PET and MRI, including developing a PET biomarker that targets and helps measure the mechanisms of pain at the molecular level. “Whether it's increased ion channels or increased pain receptors, or increased cellularity, we're looking at a number of potential markers of inflammation.” That, combined with MR imaging techniques, can provide both a molecular readout along with an anatomic diagnosis to identify where the pain is originating with great specificity and sensitivity, Dr. Biswal said.
“Another example of where conventional approaches to imaging pain just haven't been very effective, has been the use of MRI and CT to image patients with non-specific back pain,” he said. “A number of medical organizations have issued recommendations advising against lumbar MRI, mainly because it has not been very predictive or helpful in the acute setting.”
Ultimately, Dr. Biswal said, improving ways to use imaging to find the source of pain will not only help patients by improving outcomes, but will serve to improve their quality of life. “We probably all have friends or relatives who struggle with chronic pain, and get labeled as crazy or depressed," he said. “Their pain can come to dominate their existence with little hope for a cure. Now, perhaps we can help them on the route to recovery.”
MIKE BASSETT is a writer based in Holliston, Mass., specializing in health and medicine.