Machine Learning is the Next Chapter of Radiology, Not the Last
Informatics experts say deep learning will “ensure radiology’s survival.”
BY RICHARD DARGAN
April 02, 2018

Fishman
Advancements in artificial intelligence (AI) have raised a new level of possibility for the future of radiology.
News stories herald the impending takeover of the profession by computers armed with machine learning (ML) software possessing the power to recognize patterns of disease that far exceeds that of humans. But leading radiology experts insist that such a takeover is unlikely; in fact, they suggest that ML and its more sophisticated subtype, deep learning (DL), will invigorate the profession and make radiologists more vital than ever to patient care.
“One reason radiology has been so successful is that we are constantly changing,” said Elliot K. Fishman, MD, professor of radiology and oncology at the Johns Hopkins University School of Medicine in Baltimore, MD. “If anything, deep learning will guarantee our survival.”
At Johns Hopkins, Dr. Fishman helps spearhead the Felix Project, a multi-year, multi-million-dollar effort to provide earlier detection of pancreatic cancer on imaging by developing computer algorithms to read CT scans.
During the first year-and-a-half of the project, named after a potion in the Harry Potter books, multi-disciplinary researchers (radiology, pathology, genetics, computer vision), including ML expert Alan Yuille, PhD, used more than 1,000 representative normal scans to teach the computer to recognize the pancreas. For the second year, beginning last September, researchers employed some 180 scans to begin to teach the computer to recognize pancreatic cancer.
Preliminary results of the program, which exploits the fact that computers are better than humans at picking up textural shape changes in organs, have been promising.
“We are getting 60 to 70 percent accuracy in pancreatic cancer detection on test cases,” Dr. Fishman said. “This is a program that could run on every single abdominal scan in the future and help with the early detection of pancreatic cancer."
Radiologists including Linda Chu, MD, Karen Horton, MD, and Satomi Kawamoto, MD, were key to the development process, since the gold standard for AI is the radiologist. Each normal case and each case of pancreatic cancer takes approximately four hours to annotate. Without annotated data the task would be impossible.
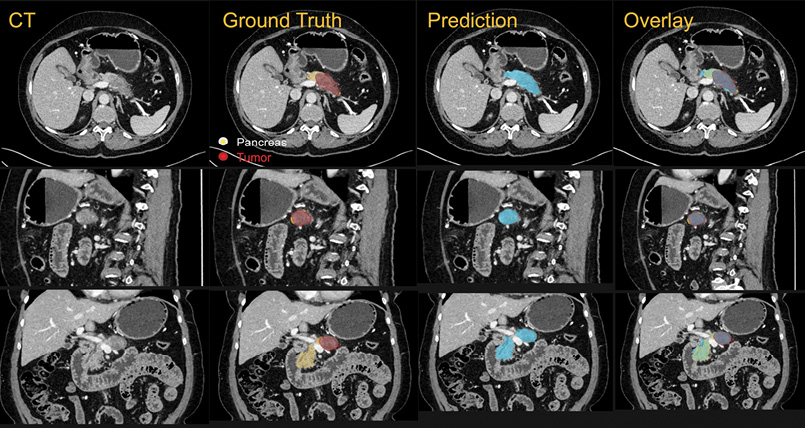
From the Felix Project at Johns Hopkins: An example of the computer's ability to recognize not only the pancreas but the pancreatic cancer. The ground truth is the radiologist and the prediction and the overlay is the computer algorithm detecting both normal gland and tumor. Note the 1-1 correlation between the radiologist and the computer prediction. All images courtesy of Johns Hopkins University School of Medicine
From the Felix Project at Johns Hopkins: An example of the computer's ability to recognize not only the pancreas but the pancreatic cancer. The ground truth is the radiologist and the prediction and the overlay is the computer algorithm detecting both normal gland and tumor. Note the 1-1 correlation between the radiologist and the computer prediction. All images courtesy of Johns Hopkins University School of Medicine
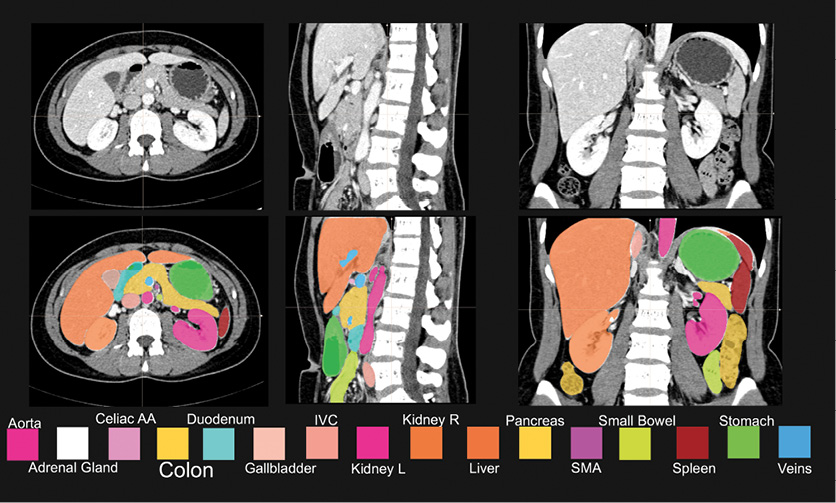
Color-coded mapping of the segmentation of the abdominal organs by radiologists to provide the information needed to train the computer deep networks.

Prevedello
AI Revolutionizing Radiology Workflow
Radiology workflow is another active area of AI research. Luciano M. Prevedello, MD, MPH, chief, division of medical imaging informatics and assistant professor of neuroradiology at the Ohio State University Wexner Medical Center in Columbus, Ohio, served as lead author on a December 2017 Radiology study that assessed the performance of an AI tool using a DL algorithm for detecting critical findings on head CT, such as hemorrhage, mass effect, hydrocephalus and stroke. (See Web Extras.)
Using more than 2,500 representative images to train the computer, Dr. Prevedello and colleagues demonstrated that the tool could one day independently screen non-contrast head CT examinations and notify the interpreting radiologist of critical findings.
“The algorithm analyzes the data set and, if it detects a critical finding, sends it to the top of the list to be read,” said Dr. Prevedello, who serves as chair of the Machine Learning Subcommittee of the RSNA Radiology Informatics Committee. “The faster you recognize an important finding, the better it is for the patient.”
ML has some clear-cut advantages over humans. It provides more consistency, Dr. Prevedello said, and is not prone to fatigue, potentially reducing error rates.
“If we consider only things we can see, then radiologists perform at a very high level of accuracy,” he said. “But imaging data contains so much information, and computers can extract features from data in a way that would be very hard for humans to replicate.”
Signs of the feverish activity in the AI-radiology arena are everywhere. For example, 2017 saw FDA approval of a self-teaching artificial neural network to help physicians diagnose heart problems and software that provides AI-assisted stroke detection for CT scans and automatically notifies neurovascular specialists by text message. A new smartphone app uses algorithms based on millions of stored images to calculate the likelihood that a mole is becoming cancerous.
“In the past, this field was evolving at a linear pace, but now we may be getting into an exponential phase of growth,” Dr. Prevedello said. “This now has the attention of people from different backgrounds, and that is one of the many reasons why the evolution is different from before."
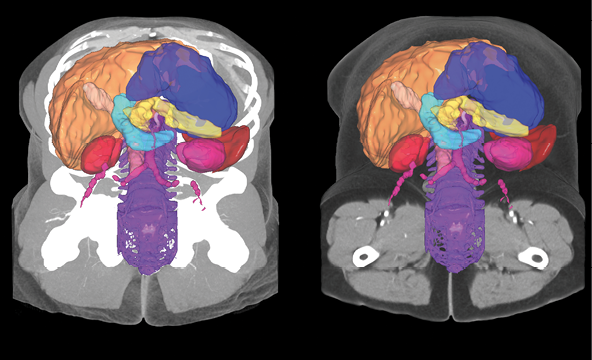
In training the computer to detect the pancreas and eventually pancreatic tumors, the Johns Hopkins team also taught the computer an algorithm to recognize all of the key abdominal structures, as shown in this multi-organ segmentation result of the abdomen.

Powell

White
Embracing ML is Key to Radiology’s Future
Kimberly Powell, vice president of healthcare at NVIDIA, a leading technology company and AI provider, attributes this evolution to the accelerating pace of three developments: more data, better algorithms and faster computation.
“We are at a turning point where we can unlock useful applications to help with radiology workflow,” she said. “With the number of imaging exams increasing, radiologists can’t spend as much time on interpretation and AI provides immediate help with that.”
Not everyone is sanguine about these developments, however. There is anecdotal evidence that concern about the future obsolescence of radiology is affecting medical students considering careers in the field.
“The fear is definitely there,” Dr. Prevedello said. “My response is that there is no question what we do today is different from what we will do in 10 years, but I say this with a lot of excitement. I feel very strongly that the solution to fear is education, and that we as the radiology community should embrace and understand ML as much as we can.”
Richard D. White, MD, chair of the Department of Radiology at the Ohio State University, points out that these pivotal moments are no stranger to radiology and compares the rise of AI with the arrival of CT in the early 70s and MRI in the early 80s.
“When CT and MRI were introduced, they improved the view of anatomy and insights into tissue properties so much that people said radiologists would no longer be needed," Dr. White said. "But these technologies actually drove the need for even more imaging and more radiologists with greater knowledge who made bigger contributions. Likewise, this new technology will provide ability to more comfortably exclude disease and detect even more findings when disease is present. And someone will need to integrate this information for our patients. Our role as clinicians will be expanded and enhanced by this technology.”
While it is difficult to quantify overall trends in radiologists' interest and investment in AI, the 2017 RSNA annual meeting offered evidence that more are getting the message.
There was a noticeable rise in attendance and interest at AI-related events at RSNA 2017 compared with the previous year. And RSNA’s first-ever Machine Learning Pavilion was packed with attendees at the 2017 meeting.
“There is an understanding in the radiology community that this technology will benefit everyone in a positive way,” Powell said. "Assisting radiologists with screening, prioritization and using algorithms to see what is difficult to the human eye are all ways AI will empower the profession of radiology."
Powell expects that over the next five years, ML will provide assistance for some of a radiologist’s simpler tasks. Beyond that, she envisions a paradigm shift, where radiologists no longer sit and type at computers but speak to instruments instead.
“The time they save will allow them to focus on the imaging that matters for patients,” Powell said.
Integrating ML with Education
Education and training are critical to moving radiology into the AI age, experts say, and programs are already taking place to help smooth that transition. More than 1,000 radiologists, IT staffers and researchers attended the DL classroom presented by NVIDIA at RSNA 2017. But education must start even earlier, according to Dr. Prevedello.
“We have an obligation to make machine learning part of our medical student and radiology resident education to prepare for the future,” he said. “In the same way we learn about artifacts generated by a defective detector on CT or noise in MRI, we will need to understand why an algorithm may produce unexpected results."
And what about those radiologists who might not be sold on ML? They could find themselves in a vulnerable position, according to Dr. Fishman.
“If you’re a radiologist and you say, ‘I’m going to close my eyes and hope this [machine learning] will go away,’ you will end up being replaced,” he said. “On the other hand, if you say, ‘I will embrace this technology and use it,’ you will not only stay employed, you will end up improving patient care.”
Web Extras
- Access the study, “Automated Critical Test Findings Identification and Online Notification System Using Artificial Intelligence in Imaging” at RSNA.org.
Editor's Picks
Imaging Meets the Forensic Files
Planes, Trains and Automobiles: RSNA 2025 Travelers Brave Chicago's Historic Snowfall - Part 3
Planes, Trains and Automobiles: RSNA 2025 Travelers Brave Chicago's Historic Snowfall - Part 2
Planes, Trains and Automobiles: RSNA 2025 Travelers Brave Chicago's Historic Snowfall